German researchers have discovered that FDG uptake in major arteries is the "strongest predictor of a subsequent vascular event" in cancer patients, with severe calcification also indicating high risk, according to an article published in the October issue of the Journal of Nuclear Medicine.
Researchers from the department of nuclear medicine at the University of Munich noted that imaging has historically been used to detect signs of atherosclerosis by measuring a cross-section of the arterial lumen to determine degree of stenosis. Although stenosis can be a sign of plaque burden, recent research indicates that inflammatory activity within plaque can also be an important predictor of plaque rupture -- and PET/CT is a good tool for detecting plaque inflammation (JNM, October 2009, Vol. 50:10, pp. 1611-1620).
A research team led by Dr. Axel Rominger wanted to determine whether PET/CT could be used to help predict vascular events in an asymptomatic population; as their study cohort, the team used a group of 1,000 patients who had received the scans for neoplastic disease. The researchers also wanted to demonstrate the value of vascular imaging in detecting incidental cardiovascular findings during oncologic investigations.
Study protocols
The researchers started with a population of 1,000 cancer patients who had been referred to their facility for PET/CT scans between August 2004 and August 2007. From this group, 68 were lost to follow-up, leaving 932 patients.
Of that group, 282 died from cancer during follow-up (mean time, 29 months), and 15 experienced nonfatal or cerebrovascular events during follow-up. For the remaining 638 patients, the researchers created a control group by randomly selecting every other PET/CT patient to produce a group of 319 patients.
All patients were imaged with FDG on a PET/CT system (Gemini, Philips Healthcare, Andover, MA) featuring a germanium oxyorthosilicate full-ring PET scanner and a two-detector-row CT device.
Patients fasted for at least six hours prior to the scan to ensure a serum glucose level below 130 mg/mL. The patients also received an intravenous injection of 200 to 480 MBq of FDG. Sixty minutes after FDG administration, data were acquired via a low-dose CT scan, which imaged the patients from the base of the skull to the proximal thighs. PET images then were acquired in 3D mode.
An experienced reviewer who was blinded to all patient or clinical information read the PET/CT results. Standardized uptake values (SUVs) for FDG were measured in both common carotid arteries, the ascending aorta, the aortic arch, the descending aorta, the abdominal aorta, and both iliac arteries.
For blood-pool SUV measurements, three regions of interest 1 cm in diameter were placed in the midlumen of the inferior and superior vena cava, and the mean of the six measurements was calculated to represent blood-pool activity. Within each region of interest, the maximal SUV was divided by the blood-pool SUV to calculate a target-to-background ratio (TBR) for each arterial segment.
CT analysis
The CT scans were analyzed for levels of calcified plaque in the walls of the same arterial segments imaged by FDG-PET. The amount of calcification was ranked on a scale beginning at zero, which indicated an absence of plaque, and increasing to four, which indicated more than 50% of plaque present within a vessel.
A target-to-background ratio of greater than 1.7 and a calcified plaque score of greater than three were used as the thresholds to identify arterial segments with increased FDG uptake, signifying heavy calcifications.
The study then analyzed a total of 2,672 arterial segments in the entire group of 334 patients (15 patients with vascular events and 319 control subjects). Of the 334 patients, 319 underwent CT with an intravenous contrast agent. The remaining 15 patients received low-dose CT with attenuation correction.
 |
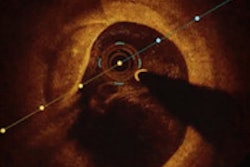
| Transaxial CT (left), FDG-PET (center), and fused PET/CT (right) of an 81-year-old male patient with significantly increased uptake in the region of the aortic arch. Calcified plaque in the aortic arch was rated as three, with a calcified plaque sum of 21. The patient experienced a myocardial infarction 14 months after the image was taken. Image courtesy of the Journal of Nuclear Medicine and the University of Munich. |
The researchers found a correlation between frequency of vascular events and patients with a target-to-background ratio ≥ 1.7 and a calcified plaque sum greater than 15. For example, 32% (9/28) of patients who had mean TBR ≥ 1.7 had cardiovascular events, compared with 2% (6/306) of patients who had mean TBR < 1.7.
For calcified plaque sum, 21% (6/28) of patients with calcified plaque sums ≥ 15 had cardiovascular events, whereas only 3% (9/306) with calcified plaque sums < 15 had events.
"The combination of a calcified plaque sum greater than 15 and a mean TBR of greater than 1.7 identified patients at highest risk for a future vascular event," the authors concluded.
Vascular events
Among the 15 patients who had a vascular event, five patients experienced ischemic strokes, seven received coronary stent implantations after acute coronary syndrome, and three had myocardial infarctions. The researchers found that patients who experienced a vascular event during follow-up were older and a greater proportion were men. Those patients also had a greater prevalence of hypertension than the study's control group.
In comparing SUVs from the blood-pool regions of interest, there was no significant difference between the two groups of patients who had received contrast and those who did not receive contrast. In addition, in a comparison of TBR, there was no difference between patients who had low-dose CT and patients who had diagnostic CT.
Based on the results, the researchers concluded that there was a "clearly higher rate of disproportional distribution patterns for FDG uptake and calcified plaque scores in the small group of patients who had a vascular event during follow-up than in those without events (62% compared with 22%)."
In addition, patients with a vascular event during follow-up showed a higher rate of increased TBR and low calcified plaque values (81%) than the control group (62%).
The study cited several limitations. Among them, the authors noted that the cancer type and chemotherapies among the cancer patients imaged by PET/CT may have been a confounding factor in the expression of vascular pathology. However, they countered that there was "no significant relationship between the main tumor types (breast, ovarian, lung, and colorectal) and either the vascular findings or concurrent vascular event risk factors."
The results of the study indicate that patients receiving PET/CT scans for diagnosis or staging of cancer could also receive atherogenic risk stratification that they otherwise would not receive, the researchers concluded. They recommended that "larger, prospective trials" of patients without cancer be conducted to substantiate "these promising results" to a broader range of patients.
By Wayne Forrest
AuntMinnie.com staff writer
October 9, 2009
Related Reading
Symptomatic patients with zero CT calcium scores still have cardiac events, October 2, 2009
CTA predicts coronary plaque instability, June 30, 2009
FDG-PET aids in detecting atherosclerosis activity, February 23, 2009
FDG-PET/CT may play role in plaque evaluation, September 12, 2008
Cedars-Sinai explores PET's future in nuclear cardiology, April 11, 2008
Copyright © 2009 AuntMinnie.com