In 2018, patients in the U.K. will have access to high-energy proton therapy on home soil, with the opening of government-funded facilities at University College London Hospitals (UCLH) National Health Service (NHS) Foundation Trust and the Christie NHS Foundation Trust in Manchester. At the College of Radiographers' Annual Radiotherapy Conference, held last week in Bristol, delegates heard about the latest developments in this ambitious project.
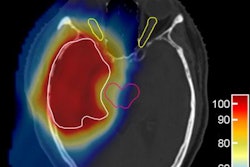
Dr. Adrian Crellin, consultant clinical oncologist and clinical lead for the National Proton Beam Therapy Service, explained the rationale for building the two new proton therapy facilities -- which between them will provide capacity to treat up to 1,500 patients per year. Proton therapy, he says, is all about reducing treatment side effects. With many pediatric cancers having high cure rates, and young patients living for long times after treatment, it's imperative to minimize the irradiation of healthy, developing tissue.
 Adrian Crellin, consultant clinical oncologist and clinical lead for the U.K.'s National Proton Beam Therapy Service.
Adrian Crellin, consultant clinical oncologist and clinical lead for the U.K.'s National Proton Beam Therapy Service.Lowering this nontarget dose can, for example, reduce the impact on a young patient's bone growth, fertility, and IQ, and could lower the risk of secondary malignancies and late effects. "It's not the conformality of the delivered dose, which IMRT [intensity-modulated radiotherapy] can do beautifully," he said. "It's the dose that you don't give to the child that matters."
Proton therapy is also an optimal treatment for selected adult cancer cases, such as skull base and paraspinal tumors, for example. In areas that are less clear cut -- such as treatment of lung and prostate cancers -- clinical trials may be required, Crellin noted. "If we pick the right patients, we can do things with protons that conventional radiotherapy just can't do," he said.
Currently, the U.K.'s only proton therapy facility is the Douglas Cyclotron at the Clatterbridge Cancer Center, which uses a 62 MeV proton beam to treat tumors of the eye. Crellin pointed out that the same cyclotron has been in use since 1989 and has now treated more than 2,000 patients with "stunning results."
For all other cases approved for proton therapy, the NHS (the U.K.'s publicly funded healthcare system) sends patients abroad for treatment in the U.S. (at the University of Florida Proton Therapy Institute in Jacksonville and the ProCure Proton Therapy Center in Oklahoma City) or at the Paul Scherrer Institute in Switzerland. To date, approximately 522 patients (377 children and 145 adults) have been approved for treatment through the NHS Proton Overseas Program.
This scheme will continue whilst the U.K. proton therapy centers are being built, and will be extended to encompass more patients. This includes treatment of more types of pediatric cancers, as well as extending the eligible age group to include older teenagers and young adults. "We are tracking the outcomes of pediatric cases; we don't expect higher cure rates, we expect lower side effects in ten years' time," Crellin said. Eligibility will also be expanded for selected groups of adult patients, such as those with advanced paranasal sinus tumors, for example, which require dose escalation.
 Design of the planned proton therapy center at the Christie.
Design of the planned proton therapy center at the Christie.Once the UCLH and Christie centers are up and running, the aim is to bring the overseas workload back to the U.K. Treatments will continue for existing approved cancer cases, and trials or formal evaluations will be performed to gather evidence for potential new indications. Crellin noted that demonstrating evidence for proton therapy is not straightforward, however, as many cancers treated with protons are rare and large randomized trials are not always possible.
Crellin rounded off his presentation by emphasizing the unusual nature of evidence associated with proton therapy studies. He pointed out that while dose modelling is an everyday tool in clinical practice, modelling evidence is excluded from NHS reviews. "We can quantify the effect of every gray to the heart, and can model the loss of IQ with radiation," he said. "To not allow this evidence is illogical, we don't use our modelling argument well enough."
The inside take
The next speakers -- Kevin Sullivan, radiotherapy services manager at UCLH, and Hazel Pennington, lead radiographer for the proton project at the Christie -- provided a joint update on their respective projects.
"It all started back in 2009," Sullivan explained when the U.K. launched a competitive process to identify possible NHS providers of high-energy proton therapy and then selected The Christie and UCLH as potential sites. In 2013, the U.K. government committed 250 million pounds (334 million euros) in funding to build the two centers, each of which will incorporate three treatment rooms.
 Kevin Sullivan, radiotherapy services manager at UCLH, and Hazel Pennington, lead radiographer for the proton project at the Christie.
Kevin Sullivan, radiotherapy services manager at UCLH, and Hazel Pennington, lead radiographer for the proton project at the Christie.The next stage was the equipment procurement, which Sullivan says was a lengthy process. Having started with a choice of 11 manufacturers, the Christie and UCLH teams have finally chosen a preferred supplier. Sullivan declined to share the details, however, as this decision is still awaiting Treasury approval.
Pennington took a look at some of the other issues arising from these new developments, including the increased workforce requirements. She noted that the yearly patient throughput for each site, about 750 patients at full capacity, is similar to the number of patients treated by two radiotherapy linacs. However, about double the number of staff will be required.
"This has been a driver for looking at the radiotherapy workforce in general," she explained. "It's really important to start recruiting early. The recruitment plan is being matched against the equipment commissioning schedule and the two-year ramp up." There is also a need to expand the skills base of new recruits, a process that will include onsite vendor training and overseas visits, as well as study days, MSc modules, and e-learning programs.
Pennington took a look at typical working day for the new proton therapy centers, noting that the imaging and overall workflow will be similar to that currently used for photon-based radiotherapy. Due to the larger proportion of children being treated, however, more general anesthesia will be required. Overall, she predicted 14-hour clinical days for treatment delivery, with "physicists working into the night to perform patient-specific QA and maintenance."
The focus now is on construction of the two new facilities. "There will be a lot of concrete," Pennington said, noting that the Christie is sited in a highly residential area, which can complicate large construction projects. Sullivan highlighted some different challenges for UCLH, which is located right in the center of London. Site construction will entail digging 30 m deep. "We've been told officially that we'll be building the deepest, widest hole in London," he said.
"The final business case has now been approved by both trusts and is with the treasury for the final sign off," Sullivan added. "We are aiming to treat first patients in 2018 -- in April or May at the Christie and November or December at UCLH."
© IOP Publishing Limited. Republished with permission from medicalphysicsweb, a community website covering fundamental research and emerging technologies in medical imaging and radiation therapy.