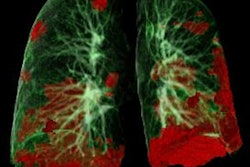
With the COVID-19 pandemic now in at least a fourth wave, physicians have a better understanding of how the disease affects the body beyond the lungs -- including the kidneys. Experts shared their knowledge and experiences on 2 March at the ECR 2022 Overture.
In a session titled "COVID-19 in the GU tract: What do we know today?" a panel of three specialists described how imaging can be used to track kidney complications in COVID-19 patients.
"COVID-19 is a disease that started mainly as a chest issue," said session moderator Prof. Lorenzo Derchi of the University of Genoa in Italy. "However, it has been shown to be a multiorgan disease, and acute or chronic kidney injury is often seen in these patients."
The panel included Dr. Alberto Tagliafico of the University of Genoa in Italy; Prof. Mathias Prokop, PhD, of Radboud University Medical Center in Nijmegen, the Netherlands; and Prof. Marie-France Bellin, of University Paris Saclay.
 The three speakers and moderator discussed the latest research findings in renal imaging of COVID-19 patients during Wednesday's ECR session.
The three speakers and moderator discussed the latest research findings in renal imaging of COVID-19 patients during Wednesday's ECR session.A bird's eye view
Tagliafico gave an overview of how COVID-19 can affect the renal system and how imaging can be used to screen for potential kidney damage in these patients, citing a number of studies conducted in 2020 and 2021. He noted that there is a high prevalence of kidney involvement in COVID-19 disease which can manifest as hematuria, proteinuria, and acute kidney injury. The incidence of acute kidney injury in hospitalized COVID-19 patients is high, ranging from 5% to 37%, and it is associated with higher rates of in-hospital death.
Both contrast-enhanced and noncontrast CT can be used to diagnose kidney problems in COVID-19 patients, Tagliafico noted.
"Contrast-enhanced CT [can visualize] renal infarction, [which can be caused by] cardioembolic disease, renal artery injury, hypercoagulable states, thromboembolism and in situ thrombosis and can lead to renovascular hypertension, chronic kidney disease, and end-stage kidney disease," he said.
Dual-energy CT techniques can help identify heterogeneous enhancement of the renal cortex even in patients who aren't presenting with abnormal kidney function.
"A large proportion of patients with mild to moderate COVID had perfusion defects in their lungs and kidneys," he said.
But contrast CT should be used with caution in COVID-19 patients with possible kidney damage if contrast isn't necessarily indicated, Tagliafico warned. One study he cited found that contrast-induced acute kidney injury was observed 48 hours after imaging in 24% of COVID-19 patients.
Noncontrast chest CT may also identify COVID-19-related kidney damage, which can appear as a decrease in renal parenchymal attenuation and the presence of perinephric fat stranding in patients with COVID-19.
"Perinephric fat stranding on nonenhanced CT has been associated with renal impairment, especially in the elderly," Tagliafico said.
Assessing renal involvement
Prokop spoke about renal involvement in COVID-19, noting that during the first wave of the pandemic, clinicians were identifying kidney injury in more than 30% of patients hospitalized for the disease -- and about 50% of these patients required dialysis.
The SARS-CoV-2 virus damages the kidneys in a variety of ways, including the following, according to Prokop:
- Direct cytotoxic damage by infection
- Secondary fibrosis after infection
- Cytokine-induced hyperinflammatory states (cytokine storms)
- Microvascular injury
- Prothrombotic state in COVID-19 (thrombosis, emboli)
- Associated hypovolemia, hypoxemia
- Nosocomial sepsis
But it can be challenging to distinguish COVID-19-related kidney complications from non-COVID-19 ones, Prokop noted.
 Prof. Mathias Prokop, PhD.
Prof. Mathias Prokop, PhD."[For example] renal infarcts caused by COVID-19 are similar to those found in non-COVID-19 patients," he said.
Which imaging modality is best for diagnosing kidney injury in COVID-19 patients? It depends on whether the individual has renal functional impairment or not, since CT contrast can aggravate or even prompt acute kidney injury, according to Prokop.
"If there's no renal functional impairment, ultrasound or contrast-enhanced CT can be used," he said. "[But] if there is renal functional impairment, ultrasound is the first modality to use, unless something is life-threatening [and contrast is indicated]."
Is the patient fragile?
Bellin discussed the need to assess the "fragility" of COVID-19 patients when it comes to deciding how best to diagnose kidney injury caused by the illness. Fragile patients are those with chronic or end-stage kidney disease, those with kidney transplants, older individuals with multiple comorbidities, and those who are immunocompromised (due to cancer treatment, for example).
Bellin offered a variety of statistics from studies conducted between 2020 and 2021 that confirms how patient fragility influenced COVID-19 outcomes:
- During the first wave of COVID-19, the mortality rate for patients who also had acute kidney injury ranged from 10% to 14%; of these, only 30% survived and recovered normal renal function.
- COVID-19 patients with end-stage kidney disease had a risk of hospital death of 31.7%, compared with 25.4% among those who did not.
- COVID-19 patients who also had kidney transplants had higher rates of mortality, at 30% compared with 25%; acute kidney injury was present in 30% to 89% of hospitalized COVID-19 kidney transplant patients.
- COVID-19 patients with cancer had higher mortality risk, at 28.6%, compared with 2.3% for all patients with COVID-19.
Bellin concluded with some suggestions on how to care for COVID-19 patients who are also at risk of kidney injury.
"Be prepared to perform bedside renal ultrasound and contrast-enhanced ultrasound in patients with renal insufficiency and be aware of numerous complications that can develop in fragile patients related to COVID or immunosuppression," she said. "Prompt diagnosis will facilitate appropriate care."