U.K. researchers are recommending the use of PET/MRI to assess suspected cases of cardiac sarcoidosis, with late gadolinium enhancement and FDG uptake as the key indicators of disease, according to a study published online on 8 January in the European Heart Journal.
The hybrid imaging modality also can help identify patients who are at greatest risk of death, arrhythmia, and heart failure, as clinicians investigate disease activity and a patient's prognosis.
"We have shown this approach improves diagnostic sensitivity and the ability to risk-stratify patients according to the presence of scar and inflammation," wrote lead author Dr. Eleanor Wicks, from the University College London Institute for Cardiovascular Science and Barts Heart Centre at St. Bartholomew's Hospital in London. "The lower specificity of hybrid PET/MRI compared with performing PET or late gadolinium enhancement on cardiovascular MR alone likely reflects the capability of the technique to detect preclinical stages of disease."
Sarcoidosis diagnosis
Cardiac sarcoidosis is an inflammatory disorder in which approximately 5% of patients experience overt cardiac involvement, according to previous research. On the other hand, past studies also show at autopsy that 50% of those cases with cardiac involvement are fatal. The rate suggests that "cardiac sarcoidosis is frequently underdiagnosed with potentially life-threatening consequences," Wicks and colleagues wrote.
Currently, the gold standard to diagnose cardiac sarcoidosis is through an endomyocardial biopsy, but the invasive procedure can be risky, and results are often inconclusive due to the spread of lesions in the basal, lateral, and epicardial segments of the left ventricle wall. Therefore, the researchers sought to assess the combined capabilities of FDG uptake in PET images to noninvasively visualize myocardial inflammation and late gadolinium enhancement in cardiovascular MRI to view postinflammatory myocardial scarring.
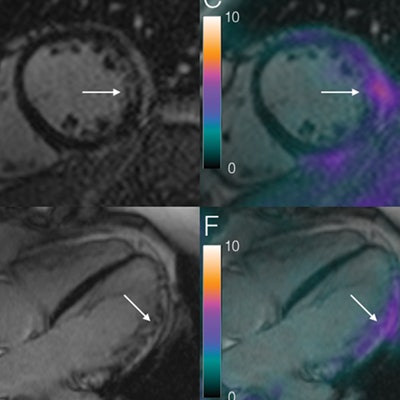
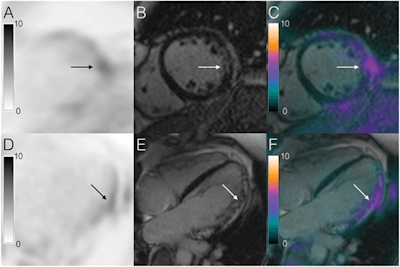 Images show concordant late gadolinium enhancement compared with FDG uptake on PET/MRI in a patient with biopsy-proven cardiac sarcoidosis. Images A to F illustrate short- and long-axis imaging of a concordant pattern of overlying inflammation and late gadolinium enhancement (fibrosis). Images A and D illustrate lateral FDG uptake (arrow), along with patchy epicardial and midmyocardial late gadolinium enhancement (images B and E; arrow). When fused (images C and F), the images offer an overlay of late gadolinium enhancement and FDG uptake (arrow highlighting the area of abnormality). Images courtesy of the European Heart Journal.
Images show concordant late gadolinium enhancement compared with FDG uptake on PET/MRI in a patient with biopsy-proven cardiac sarcoidosis. Images A to F illustrate short- and long-axis imaging of a concordant pattern of overlying inflammation and late gadolinium enhancement (fibrosis). Images A and D illustrate lateral FDG uptake (arrow), along with patchy epicardial and midmyocardial late gadolinium enhancement (images B and E; arrow). When fused (images C and F), the images offer an overlay of late gadolinium enhancement and FDG uptake (arrow highlighting the area of abnormality). Images courtesy of the European Heart Journal."The development of hybrid PET/MRI offers an efficient combined method for performing simultaneous structural, functional, and tissue characterization with cardiovascular MR and metabolic imaging with PET," the study authors noted.
The group looked at 51 consecutive patients, with a median age of 50 years (± 13 years) and known or suspected cases of cardiac sarcoidosis between April 2012 and July 2013. Among the subjects, 44 (86%) patients had suspected cardiac sarcoidosis and histologically proven extracardiac sarcoidosis, while seven (14%) cardiac sarcoidosis cases were confirmed through endomyocardial biopsy.
All patients underwent a whole-body PET/MRI scan on a hybrid system with a 3-tesla MRI system (Biograph mMR, Siemens Healthineers). The PET protocol included intravenous injection of 370 MBq of FDG at a mean of 64 minutes (±13 minutes) prior to PET/MRI image acquisition. Standard cardiac MRI was performed to evaluate late gadolinium enhancement simultaneously with FDG-PET acquisition following single breath-hold attenuation correction.
Two experienced readers who were blinded to the clinical data of each patient interpreted the FDG-PET and contrast-enhanced MR images by consensus.
The researchers also followed the patients for a median of 2.2 years to record their outcomes. The primary end point was death, aborted sudden cardiac death, sustained ventricular arrhythmia, complete heart block, and hospital admission for heart failure. Secondary endpoints included a fall in left ventricular ejection fraction (LVEF) of more than 10%, ventricular tachycardia, or hospital admission for another cardiac-related event.
Modality comparisons
In reviewing the PET and MR images together and individually, the readers identified 28 patients who showed abnormal cardiac PET findings (17 focal and 11 focal on diffuse uptake), while the other 23 cases (45%) showed negative cardiac PET findings (19 had no cardiac uptake and four patients had a diffuse pattern).
When the two modalities were combined, 17 (33%) patients displayed abnormalities in both PET and cardiovascular MRI. In addition, 15 (29%) subjects showed abnormalities on late gadolinium enhancement only, 11 (22%) patients had only PET abnormalities appear, and eight (16%) patients showed no abnormalities at all.
Interestingly, while PET/MRI exceeded PET and MRI alone for sensitivity in detecting cardiac sarcoidosis, the hybrid imaging modality fell short for specificity.
"The lower specificity of hybrid PET/MRI compared with performing PET or late gadolinium enhancement on cardiovascular MR alone likely reflects the capability of the technique to detect preclinical stages of disease," the authors wrote.
| PET, MRI, and PET/MRI to detect cardiac sarcoidosis | |||
| FDG-PET alone | MRI alone | PET/MRI | |
| Sensitivity | 60% | 82% | 94% |
| Specificity | 56% | 78% | 44% |
| Positive predictive value | 71% | 87% | 76% |
| Negative predictive value | 44% | 79% | 80% |
Abnormalities seen on both PET and MRI also proved to be the strongest predictor of major adverse cardiac events. Based on a median follow-up of 2.2 years, 18 patients (35%) experienced an adverse cardiac event, 16 of which were the more serious primary end points, compared with two cases of less serious secondary end points.
"Simultaneous PET/MR is an accurate method for diagnosing cardiac sarcoidosis," the authors concluded. "FDG-PET and cardiovascular MR combined offers complementary information on disease pathophysiology. PET and cardiovascular MR should therefore be considered in the assessment of disease presence, stage, and prognosis in cardiac sarcoidosis."
Wicks and colleagues noted several limitations to the study, including the absence of a PET perfusion evaluation, because it would have meant additional radiation dose for patients.
"Moreover, the local protocol for [cardiac MR] did not include perfusion assessment as routine, and as most patients had previously undergone coronary angiography, this was excluded from the protocol," they added.
The researchers also recommended additional studies to validate the potential of PET/MRI to guide and monitor patient treatment.