Clinicians can reduce a standard dose of FDG by as much as 90% and still achieve clinically acceptable PET image quality in time-of-flight (TOF) PET/MRI scans for breast cancer, according to a Swiss study published online on 7 June in the Journal of Nuclear Medicine.
One benefit from the reduction in FDG dose is less radiation exposure to a patient. In addition, the decrease in radiation burden might justify partial-body PET/MRI scans for certain dedicated indications, the researchers contend.
"The possibility to reduce the amount of injected tracer for specific indications will significantly reduce the radiation burden of patients, which may result in a paradigm shift in PET imaging," said lead author Dr. Bert-Ram Sah from the department of nuclear medicine at the University Hospital of Zurich. "Based partly on significant radiation burden, PET imaging in oncology is often restricted to whole-body examinations in patients with different cancer indications. With the results of this study, this restriction might potentially be reconsidered."
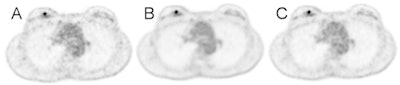 A 49-year-old patient with an invasive breast cancer. The FDG-avid, 8-mm lesion is shown in the axial image on the right side. The patient was injected with 218 MBq of FDG (body weight of 73 kg) A: Two-minute TOF, B: 100% of FDG dose, C: 44 MBq (20% dose), D: 22 MBq (10% dose), E: 11 MBq (5% dose), F: corresponding contrast enhanced MRI image. For a PET/MRI examination with the images shown in D, this patient would receive an estimated radiation burden of 0.44 mSv. All images courtesy of Dr. Bert-Ram Sah.
A 49-year-old patient with an invasive breast cancer. The FDG-avid, 8-mm lesion is shown in the axial image on the right side. The patient was injected with 218 MBq of FDG (body weight of 73 kg) A: Two-minute TOF, B: 100% of FDG dose, C: 44 MBq (20% dose), D: 22 MBq (10% dose), E: 11 MBq (5% dose), F: corresponding contrast enhanced MRI image. For a PET/MRI examination with the images shown in D, this patient would receive an estimated radiation burden of 0.44 mSv. All images courtesy of Dr. Bert-Ram Sah.Radiation exposure
With modalities such as PET and CT, patients are exposed to ionizing radiation. The marriage of PET with MRI has lessened the radiation burden significantly, especially with addition of the time-of-flight (TOF) imaging sequence, which has been shown to improve cancer detection through enhanced image signal to noise.
Sah and colleagues are quite familiar with the issue of reducing dose in molecular imaging scans. Study author Dr. Patrick Veit-Haibach, associate professor of molecular imaging at Toronto General Hospital, and Dr. Tetsuro Sekine, also from the University Hospital of Zurich, have published papers on dose reduction in whole-body FDG-PET/MRI scans.
"In the current trial, we wanted to extend our knowledge from this whole-body evaluation into single-station imaging," noted Sah in an email to AuntMinnieEurope.com. "Because the MRI time in PET/MRI is very often the time limiting factor -- and not the PET -- we wanted to evaluate how low we safely could reduce the radiation burden to the patient with the new detectors available."
In addition, advances in PET technology, implementation of TOF in MRI-compatible silicon photomultiplier PET detectors, and developments in reconstruction algorithms and computing also have contributed greatly to achieving the results presented in this study, he added.
Image reconstruction
In this study, the researchers analyzed 26 consecutive female patients (median age, 51; range, 34 to 83 years old) with confirmed breast cancer. The majority of patients (19 women, 73%) had invasive breast cancer of no special type. The group analyzed 71 different lesions, each of which were reconstructed five times, making a total of 355 lesions (JNM, 7 June 2018).
 Dr. Bert-Ram Sah.
Dr. Bert-Ram Sah.Prior to PET/CT, patients received 3 MBq of FDG per kilogram of body weight if they weighed 85 kg or less, while patients heavier than that received 3.5 MBq per kilogram. Approximately one hour after injection, clinical oncologic images were acquired on a PET/CT system (Discovery 690 TOF PET/CT, GE Healthcare)
PET/MRI scans were performed on a simultaneous TOF scanner (Signa PET/MR, GE Healthcare) with no additional injection of FDG. The time difference between the two hybrid scans was 38 minutes (± 3.5 minutes).
To enhance image quality, the researchers reconstructed the 20-minute PET frame for each patient in five different sets. They began with a reconstruction of the first two minutes of PET scanning time with three iterations and 28 subsets for reference and comparison. Next were reconstructions using 100% of injected FDG dose, followed by simulations based on 20%, 10%, and 5% of the original FDG dose all from the 20-minute image acquisition time.
"This way, the total scan time remains 20 minutes, and, as a result, the data still includes normal effects such as decay, biodistribution, and eventual patient motion," the authors wrote.
Two experienced nuclear medicine physicians/radiologists then interpreted a total of 130 reconstructed PET datasets among the 26 patient studies with five different reconstructions each.
Readers' ratings
In reviewing the five image datasets and their parameters, the readers rated all images good to excellent. As one might expect, the best results were obtained from PET images acquired at the 20-minute mark with 100% dose.
However, most important, image reconstruction using the full 20 minutes and 20% and 10% dose, respectively, produced better PET images than the two-minute reconstruction, with no significant differences in primary lesion detectability. Image reconstruction at 5% dose was deemed inferior to the two-minute reconstruction. However, no significant differences were found in primary lesion detectability.
| Readers' ratings for image quality based on reconstructions and dose amounts | ||||||||
| Image reconstruction measures | Mean general image quality & artifacts | p-value** | Mean image sharpness | p-value | Mean noise | p-value | Mean lesion detectability | p-value |
| At 2 minutes | 1.84 (± 0.6) | 2.28 (± 0.6) | 2.16 (± 0.6) | 1.46 (± 0.7) | ||||
| At 20 minutes | ||||||||
| 100% dose | 1.08 (± 0.4) | < 0.001** | 1.12 (± 0.3) | < 0.001** | 1.04 (± 0.2) | < 0.001** | 1.03 (± 0.2) | 0.038 |
| 20% dose | 1.32 (± 0.6) | < 0.001** | 1.64 (± 0.7) | < 0.001** | 1.44 (± 0.5) | < 0.001** | 1.14 (± 0.4) | 0.257 |
| 10% dose | 1.40 (± 0.6) | < 0.001** | 1.76 (± 0.7) | < 0.001** | 1.48 (± 0.6) | < 0.001** | 1.28 (± 0.6) | 0.763 |
| 5% dose | 1.88 (± 0.5) | 0.317 | 2.60 (± 0.8) | 0.005 | 2.28 (± 0.5) | 0.180 | 1.62 (± 0.8) | 0.142 |
**Statistically significant results. All other results not statistically significant.
Radiation exposure
When patients are injected with the full 225.8 MBq (± 55 MBq) dose of FDG, the resulting whole-body radiation burden is estimated at 4.5 mSv (± 1.1 mSv). Thus, if image quality is essentially the same for the detection of cancer-related breast lesions at reduced doses of FDG, radiation exposure to patients can be reduced accordingly.
| Estimated radiation dose exposure from FDG | ||||
| Total injected dose | 20% injected dose | 10% of injected dose | 5% of injected dose | |
| Whole-body radiation | 4.5 mSv (± 1.1 mSv) | 0.9 mSv (± 0.2 mSv) | 0.5 mSv (± 0.1 mSv) | 0.2 mSv (± 0.1 mSv) |
While the process to reduce FDG dose and maintain image quality might appear complicated, the authors noted the technique is reproducible.
"We published all details about the imaging protocol to make it easy for anyone to replicate our results, contribute to research of breast cancer imaging with comparable and advanced studies, and finally hopefully implement it into specific areas of clinical care," Sah said. "The only technical requirement is the state-of-the-art PET/MRI scanner, which is obviously not very common yet and mainly only implemented in major academic institutions."
The next step for the authors is to create a specific breast cancer/single-station imaging trial to evaluate the clinical performance, as well as areas of specific medical need, for such an imaging approach.
"Implementation into standard clinical care will, therefore, take some time, also because of reimbursement policies of health insurance companies," he continued. "Before PET/MRI can be implemented into the assessment of breast cancer, further prospective studies in a collective of patients with unclear breast lesions have to be undertaken."
Study disclosures
GE Healthcare provided financial support for the study and GE employees were among the study's authors. Only non-GE employees had control of inclusion of the data and information that might present a conflict of interest, according to the authors.



















