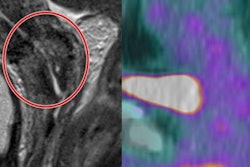
PET/MRI can become an increasingly valuable modality for the early-stage diagnosis of cervical cancer, especially when the disease spreads to the parametrium, according to a study published on 17 July in the European Journal of Radiology.
The authors combined FDG-PET with a T2-weighted MR imaging voxel segmentation method and gray-level adjustments to significantly improve accuracy, sensitivity, and negative predictive value, compared with MRI alone, in diagnosing and staging parametrial infiltration (PMI) in cervical cancer.
"With the advent of combined PET/MRI, a more precise diagnosis and staging of tumors in various parts of the body became possible, especially for women with cervical cancer," wrote the group led by Tong Wang from Shengjing Hospital of China Medical University. "PET/MRI accurately obtains anatomical and functional imaging information in real-time. Dual-modality imaging can share the same region of interest, is more sensitive and accurate than conventional single-modality imaging, and can reduce the radiation dose and examination time required."
Increasing incidence
The incidence of cervical cancer is on the rise, with approximately 85% of new cases occurring in developing countries, making it the third most common gynecological cancer in the world. Early diagnosis and accurate staging have become increasingly important, as new cervical cancer cases are trending toward younger ages.
When cervical cancer is discovered in its early stages, five-year survival rates can be as high as 95% with surgery. The catch is the potential need to remove parametrial tissue, which increases the likelihood of complications from the invasive procedure and can adversely affect a patient's quality of life.
"Accurate preoperative judgement as to the depth and extent of PMI (including parametrial soft-tissue involvement, parametrial lymph node metastasis, and intravascular tumor thrombus) is therefore crucial in assessing indications for surgery, especially for those patients above stage IIB [cervical cancer] who did not undergo surgical treatment and were treated instead with radiotherapy and chemotherapy," Wang and colleagues wrote.
These types of cervical cancer cases could benefit from the hybrid modality, which provides "more precise diagnosis and staging of tumors in various parts of the body," the authors added. MRI offers advantages such as high soft-tissue resolution, while PET has shown high sensitivity and specificity for small or concealed malignant lesions.
This retrospective study included 79 patients (median age, 53 years; range, 23-78 years) with stage IB to IIB cervical cancer. Of the total, 37 patients (47%) had postoperatively confirmed PMI and 42 (53%) had no evidence of PMI. The subjects did not undergo radiotherapy and chemotherapy before surgery. FDG-PET and MRI scans (Signa PET/MRI, GE Healthcare) were performed simultaneously from the iliac bone to the proximal femur within two weeks prior to surgery.
The MRI protocol included T1- and T2-weighted imaging, as well as 3D high-resolution T2-weighted imaging. Regions of interest (ROIs) at the largest tumor level were delineated on T2-weighted imaging, with the ROI applied to the PET image of the corresponding layer. The researchers then used a voxel-based segmentation method and adjusted gray-level calculations in the parauterine area to quantitatively analyze PET and MR results to determine if the diagnostic accuracy for PMI could be improved.
"The diagnosis of PMI with MRI or PET/MRI is mainly based on morphological observations without actual quantification, which is not optimal," Wang and colleagues wrote. "Therefore, we sought to increase the diagnostic accuracy by calculating the gray-level values of the parametrial area of PET images. ... Our calculation of gray-level values was within the same predefined [maximum] standardized uptake value (42% SUVmax) contour threshold (usually approximately 40%)."
Diagnostic accuracy
Their approach proved fruitful, with the combination of PET/MRI and gray-level adjustments achieving the best results, compared with PET/MRI and MRI alone. In fact, PET/MRI with gray levels was statistically significantly greater than MRI alone for sensitivity, negative predictive value, and accuracy.
| Diagnosis of early-stage cervical cancer with PMI | ||||
| PET/MRI and adjusted gray levels | PET/MRI | MRI | p-value* | |
| Sensitivity | 84% | 65% | 60% | < 0.05 |
| Specificity | 91% | 91% | 88% | NS |
| Positive predictive value | 89% | 86% | 82% | NS |
| Negative predictive value | 86% | 75% | 71% | < 0.05 |
| Accuracy | 87% | 79% | 75% | < 0.05 |
NS = Not statistically significant.
Based on the results, the researchers concluded that PET/MRI can feasibly evaluate PMI by combining voxel-based segmentation with gray-level calculations to improve accuracy, sensitivity, and negative predictive value.
"PET/MRI has emerged as the favorable modality in terms of scan time required since PET/MRI can simultaneously acquire MR and PET data, which reduces scanning time," Wang and colleagues noted. "PET/MRI has clear advantages in gynecological tumor evaluation, staging, and individualized diagnosis and treatment planning, especially where there is lymph node metastasis and extrapelvic infiltration."