Using PET/CT scans to assess response to therapy can help patients with head and neck cancer avoid invasive post-treatment surgery to remove any remaining cancer cells, according to a U.K. study published online 23 March in the New England Journal of Medicine.
Researchers found that 81% of patients who underwent a PET/CT scan after chemotherapy avoided neck dissection surgery, compared with only 22% of patients who were imaged with CT or MRI and avoided the operation.
"PET/CT surveillance resulted in far fewer operations, with approximately 80% of patients being spared neck dissection, and was more cost-effective than planned neck dissection over the trial period," the authors wrote (NEJM, 23 March 2016).
Only surgery option
Under previous protocols, head and neck cancer patients had little or no choice but to undergo neck dissection surgery after treatment, because there was no reliable way to identify which patients still had lingering cancer cells, according to lead author Dr. Hisham Mehanna, PhD, from the Institute of Head and Neck Studies and Education (InHANSE) at the University of Birmingham, and colleagues.
Such a procedure generally involves a three-hour operation and carries both considerable morbidity and a potential hospital stay of as long as one week to recover.
FDG-PET/CT is well-known for identifying both structural and metabolic abnormalities in tumors. One published meta-analysis reported that FDG-PET/CT achieved negative predictive values of 94% to 96% among head and neck squamous cell cancer patients after treatment.
"However, as yet there is no prospective randomized evidence in a multicenter setting to support routine adoption of this [PET/CT] approach," Mehanna and colleagues wrote.
Therefore, their goal was to compare planned neck dissections with PET/CT-guided surveillance of patients with advanced (N2-N3) nodal disease.
Study parameters
A total of 564 patients were recruited between October 2007 and August 2012 from 37 head and neck treatment centers in the U.K. for the prospective study. The mean age of the participants was 58 years, with the majority of patients being male (82%) and having oropharyngeal cancer (84%). The majority of subjects (78%) had N2a or N2b nodal disease, and 74% of the people were either current or past smokers.
Each participating center was asked whether a patient was scheduled for a neck dissection, which would be performed before (within four weeks) or after (within four to eight weeks) completion of chemoradiotherapy.
Researchers randomly divided the cohort in two groups. There were 282 patients who received a scheduled neck dissection, which served as a control group, and 282 individuals who underwent PET/CT 12 weeks after they completed chemoradiotherapy and served as the experimental surveillance group. (Two patients in the second group were later found to be ineligible for the study.)
Twelve weeks after their last cancer treatment, patients assigned to the planned neck dissection group were scanned using CT or MRI, while subjects in the experimental, surveillance group underwent PET/CT scans to assess the results of therapy.
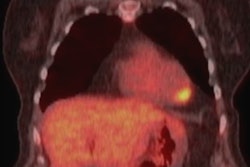
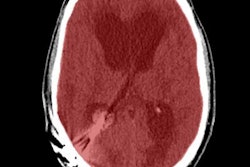
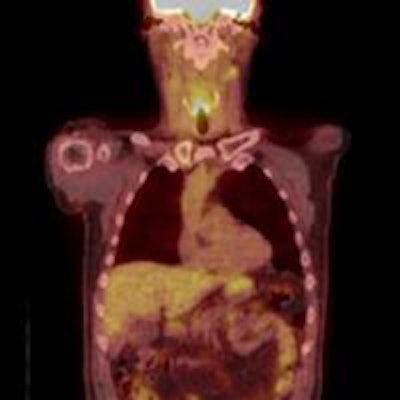
 PET/CT scans show the remaining surviving cancer cells after treatment. Images courtesy of University of Birmingham.
PET/CT scans show the remaining surviving cancer cells after treatment. Images courtesy of University of Birmingham.Patients who had significant FDG uptake on PET/CT scans after 12 weeks of treatment were classified as having an incomplete nodal response, while mild or no FDG uptake in enlarged nodes or mild FDG uptake in normally sized nodes was considered an equivocal response. These patients subsequently underwent neck dissection. All other results were deemed complete responses to therapy.
Patients also received follow-up clinical exams and imaging for at least 24 months, with suspected recurrences assessed through biopsy and pathology. Complications from surgery were recorded for 30 days after the operation, and serious adverse events were reported up to three months after a patient's last treatment.
To perform a cost analysis, researchers asked participating facilities to answer questionnaires to determine patient quality-adjusted life years (QALYs), which were combined with costs to calculate cost-effectiveness.
Outcome measures
In comparing outcomes among patients in the experimental surveillance group and those in the neck dissection group, the researchers found fewer surgical interventions in the group that underwent PET/CT imaging. There were 54 neck dissections (19%) performed within the PET/CT-guided surveillance cohort, compared with 221 such procedures (78%) in the group scheduled for neck dissection.
In addition, the PET/CT approach saved money. An analysis of the numbers indicated that PET/CT-guided surveillance was cost-effective over the two-year minimum follow-up period with a per-person cost saving of approximately 1,492 pounds ($2,190) and an additional 0.08 patient QALYs, compared with patients who had scheduled neck dissections.
But how did using PET/CT to avoid surgery affect patient outcomes? To answer this question, researchers followed patients for up to five years, with a median of 36 months, and followed 520 (92%) subjects for at least two years.
Overall, 122 patients died during that time, with a fairly even distribution of 60 deaths in the imaging-based surveillance group and 62 deaths in the planned neck dissection group. Two-year overall survival was 85% for the PET/CT-guided surveillance group, compared with 82% for the scheduled neck dissection group, indicating that the two follow-up methods had relatively similar outcomes.
Based on the results, Mehanna and colleagues concluded that the use of PET/CT scans for image-guided surveillance means that routine post-treatment surgery may no longer be necessary, and appropriate follow-up therapy can target the 20% of patients who still have persistent cancer.
The authors cautioned that their findings on the relative efficacy and cost-effectiveness of CT were based on past literature, and PET/CT-based approaches require further evaluation.
"At the time of inception of this study, it was not possible to calibrate standardized uptake values (SUV) between different scanning systems," they noted. "Interpretation of results presented here is, therefore, limited by the fact that we could not undertake assessments of SUVs in deciding on response to therapy."
Now that calibration between systems is "feasible," they added, "we are undertaking retrospective evaluation of SUVs to assess whether this improves accuracy of response assessments."
The research was funded by the U.K. National Institute for Health Research Health Technology Assessment Programme.