Lung cancer researchers from Italy have found that FDG-PET/CT is "highly sensitive" in the diagnosis of indeterminate nodules, as well as nodules larger than 15 mm and solid nodules, but less effective with other smaller, subsolid nodules.
The findings come from patients who volunteered for the Continuous Observation of Smoking Subjects (COSMOS) study, one of the largest research initiatives, which evaluated the efficacy of low-dose CT screening on high-risk smokers.
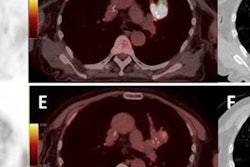
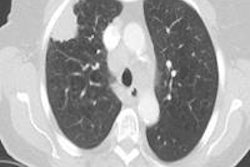
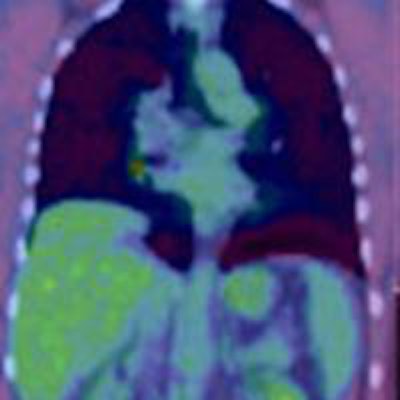
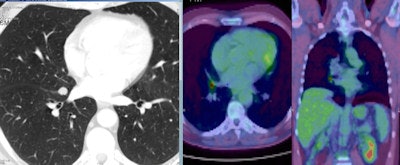 A 56-year-old man with a small nodule identified at low dose CT scan between the middle and right lower lobe. PET scan shows a high FDG uptake. A robotic segmental resection of the nodue was performed with a frozen section that showed a small cell lung cancer. Patient was treated with chemo and radiotherapy with success. Image courtesy of Dr. Giulia Veronesi.
A 56-year-old man with a small nodule identified at low dose CT scan between the middle and right lower lobe. PET scan shows a high FDG uptake. A robotic segmental resection of the nodue was performed with a frozen section that showed a small cell lung cancer. Patient was treated with chemo and radiotherapy with success. Image courtesy of Dr. Giulia Veronesi.The study authors, led by Dr. Giulia Veronesi, director of the Lung Cancer Early Detection Unit at the European Institute of Oncology in Milan, noted that CT screening for lung cancer remains up for debate. Although the National Lung Screening Trial found that low-dose CT reduced lung cancer mortality by about 20%, the modality results in a high rate of indeterminate and false-positive nodules.
"Low-dose CT screening for lung cancer can reduce lung cancer mortality, but overdiagnosis, false positives, and invasive procedures for benign nodules are worrying," they wrote. "We evaluated the utility of PET/CT in characterizing indeterminate screening-detected lung nodules."
COSMOS data
Back in 2004 and 2005, some 5,203 asymptomatic current or former smokers with a mean age of 57.7 years volunteered for the COSMOS study. Included in the cohort were ex-smokers who had quit the habit for no more than 10 years. The study excluded individuals who quit smoking within the previous five years and had malignant disease (European Respiratory Journal, online article, September 26, 2014).
CT scans were performed on a multidetector system (High/Light Speed Advantage, GE Healthcare) with no contrast. PET scans (Discovery LS, GE Healthcare) took place approximately 50 minutes after FDG injection.
As part of the diagnostic protocol, the larger the noncalcified nodules, the more often the patients received low-dose CT. Noncalcified nodules 5 mm or less in size received repeat low-dose CT a year later, while noncalcified nodules between 5.1 mm and 8 mm underwent repeat low-dose CT three months later.
Solid or partially solid nodules 8 mm or larger received FDG-PET/CT unless they were benign and were followed up with low-dose CT a year later. Baseline nonsolid nodules between 5.1 mm and 8 mm had repeat low-dose CT six months later, as did nodules larger than 8 mm.
Diagnostic criteria
Researchers considered solid nodules to be malignant if they had a maximum standard uptake value (SUVmax, corrected for body weight) of greater than 2.0 and nonsolid nodules had a SUVmax greater than 1.5.
After study criteria were applied, Veronesi and colleagues focused on 383 FDG-PET/CT scans, which were used to diagnose suspected primary lung cancer in 351 volunteers.
Also in the study were 241 suspicious nodules, which received CT-guided biopsy or surgery, which, in turn, found 196 malignant nodules and 45 benign nodules. Of that total, 142 nodules were investigated additionally with low-dose CT and determined to be benign after at least 24 months. Ten patients had multiple PET scans for various reasons.
In the analysis of the data, FDG-PET/CT showed that it was able to tell the difference between malignant and benign nodules at baseline and with nodules at least 15 mm in size. (See chart)
| FDG-PET/CT | Malignant nodules | Baseline-detected nodules | Nodules > 15 mm |
| Sensitivity | 64% | 82% | 87% |
| Specificity | 89% | 92% | 73% |
| Accuracy | 76% | 88% | 82% |
Performance, however, was significantly lower for nodules reviewed with annual scans, as sensitivity ranged between 30% and 71%, compared with baseline sensitivity of 82% and nonsolid nodules sensitivity of 79%.
When researchers evaluated size and density of nodules together, FDG-PET/CT sensitivity was poor at 21% for subsolid nodules smaller than 15 mm, compared with sensitivity of 64% for intermediate subsolid nodules between 10 mm and 15 mm.
Sensitivity for solid nodules smaller than 15 mm was 65% and 98% for solid nodules at least 15 mm in size and larger.
Veronesi and colleagues said the most relevant findings for the use of FDG-PET/CT are based on nodule size and type. For example, sensitivity was 98% for solid nodules at least 15 mm in size, "so a positive finding is almost always cancer," the study stated.
Negative predictive value was 95%, which would mean that "invasive procedures can be avoided when PET is negative, with low risk of delayed diagnosis. In fact, we had only one false-negative PET is this group, which was still stage I when it was diagnosed at screening a year later."
Veronesi and colleagues promoted the study's strength in that it represented the largest series of screened patients undergoing FDG-PET/CT, with almost all patients undergoing the hybrid modality before surgical resection.
They also cited a limitation that the results "may not be applicable to populations with higher rates of endemic inflammatory lung conditions than the Italian population."
With those considerations, researchers concluded that the FDG-PET/CT findings "are encouraging overall and suggest the technique has a role in the diagnostic workup of indeterminate nodules identified on low-dose CT screening."