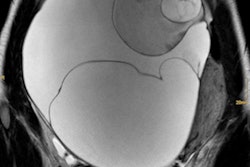
BALTIMORE - FDG-PET/CT scans can help predict disease progression and overall survival of ovarian cancer patients for as long as several years after treatment, according to a German presentation made on 9 June at the Society of Nuclear Medicine and Molecular Imaging (SNMMI) annual meeting.
Three years after completing cancer therapy, nearly two-thirds of patients with a negative follow-up FDG-PET scan were free of any disease progression, compared with less than one-fifth of patients who had a positive FDG-PET scan. Those with a negative scan also had a significantly higher rate of overall survival.
Ovarian cancer is the eighth most common malignancy among women and it carries a high mortality rate. Previous research has shown the benefits of FDG-PET/CT for diagnosis, detecting recurrence, and monitoring treatment response in cancer patients.
"But prognostic values are even more important because they are able to drive an effective therapy," lead author Dr. Federico Caobelli, from the nuclear medicine department at Hannover Medical School in Germany, told attendees. "The prognostic role of FDG-PET/CT during staging has been evaluated, but it is unclear whether the same prognostic values also pertain to the restaging process."
Caobelli and colleagues therefore sought to assess the prognostic value of FDG-PET/CT during restaging of patients with ovarian cancer, and they also explored other factors that might influence survival.
The researchers retrospectively evaluated a database of 10 nuclear medicine departments in Italy to develop a population of 168 patients with ovarian carcinoma who were between the ages of 36 and 80 years (mean age, 61.7 years). All subjects underwent restaging with FGD-PET/CT, which was performed at least six months after the completion of treatment, with the researchers noting local recurrences, nodal involvement, and distant metastases.
A follow-up FDG-PET/CT scan was performed a minimum of three years later, based on the patient's clinical information, to determine disease progression-free survival and overall survival.
FDG-PET/CT performance
Progression-free survival and overall survival were significantly longer in patients with a negative FDG-PET scan versus those with a positive scan, the researchers found.
Three years after completing treatment, 61% of patients with a negative FDG-PET scan were free of any disease progression, compared with 17% of patients who had a positive FDG-PET scan.
A negative FDG-PET scan was also associated with a significantly higher overall survival rate. Among the subjects with a negative scan, 73% were alive at three years, compared with 40% of those with a positive FDG-PET result. At five years, overall survival was 50% in the negative-scan group, compared with 18% in the positive-scan group.
"In this situation, we can see that the negativity of a PET scan is a good predictor of longer overall and progression-free survival," Caobelli said.
Local disease recurrence and nodal involvement were also linked to a greater risk of disease progression (hazard ratio = 1.8 times higher than negative studies), although the results were not statistically significant (p = 0.09). The presence of distant metastasis also increased the risk of disease progression (hazard ratio = 2.4, p = 0.003).
"We can say that FDG-PET/CT to evaluate restaging of ovarian cancer provides meaningful prognostic information, and a positive PET scan is associated with an increased risk of disease progression and reduced length of overall survival," Caobelli concluded.
The ability of a negative or positive FDG-PET scan to predict progression-free and overall survival was all the more significant because the patient cohort for the study came from 10 different Italian nuclear medicine departments, and patients underwent a variety of cancer treatments, he added.
"So even in the presence of very heterogeneous treatment, we have significant results with FDG-PET/CT," he said.
Prospective clinical trials are needed to further validate the results, but FDG-PET/CT should still be considered an important prognostic tool in the restaging process and in planning effective therapy, the researchers concluded.