When analyzing pediatric brain development on MRI scans, imaging professionals should be careful not to make assumptions based on their experiences with adult scans, urged Dr. Ellen Grant at Sunday's president's lecture at the Society for MR Radiographers & Technologists (SMRT) virtual conference. She also gave valuable career tips during the live session.
Grant urged attendees to create their own trajectories.
 Dr. Ellen Grant.
Dr. Ellen Grant."Be curious, follow your passion, dare to be different and listen to criticism; sometimes it's a good motivator, and there's always a grain of truth in everything," noted Grant. "Create teams, as science is so complicated now ... and I love to surround myself with smarter people, which makes it a rich environment and really helps us to develop science as quickly as possible. Nudge the world into a positive direction, either through our science or our interaction with colleagues."
During clinical part of her talk, she pointed out that childhood is a dynamic period of life, and the complex growth trajectories of the pediatric brain can interact with gene expression and other factors.
"What happens with these complex brain trajectories in the first thousand days sets up your cognitive function for life," noted Grant, who is director of the Fetal-Neonatal Neuroimaging and Developmental Science Center at Boston Children's Hospital.
She and her team have been trying to find ways to use imaging to capture and predict pediatric brain growth trajectories, monitor intervention, and nudge these trajectories in positive directions when they start to go awry.
However, neurological growth trajectories are hard to predict, particularly just from images, noted Grant, pointing to the need for other factors to be taken into consideration, such as Apgar scores and electroencephalograms. In an era of artificial intelligence (AI), doctors can't just use simple image-based AI approaches to predict brain trajectories in neonates, she stressed.
Evolving technology
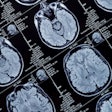
The development of new MRI hardware has helped hone diagnosis, noted Grant. In the past, imagers might see nothing on 1.5-tesla images of patients with seizures; however, the advent of phased-array radiofrequency coils has allowed them to focus on a single area of activity within the brain.
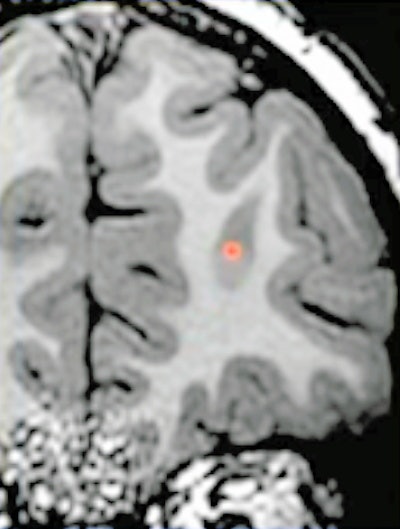 (Above) MRI shows an area of bright T1 signal indicating abnormality. (Below) A transmantle sign, a clear example of a small focal cortical dysplasia (FCD), can be visualized on the MRI. All images courtesy of Dr. Ellen Grant.
(Above) MRI shows an area of bright T1 signal indicating abnormality. (Below) A transmantle sign, a clear example of a small focal cortical dysplasia (FCD), can be visualized on the MRI. All images courtesy of Dr. Ellen Grant.Before the use of hypothermia strategies, imagers attempted to find injuries and predict outcomes with diffusion in neonates. Even when diffusion and apparent diffusion coefficient (ADC) signs similar to stroke suggested that a child's brain was damaged, MR at five months follow-up would show normal signs where there had been diffusion abnormalities, Grant stated.
"We very quickly found out that diffusion wasn't always necrosis and that diffusion didn't always evolve to these areas of cystic encephalomalacia," Grant said.
Such decreased diffusion can be seen in inflammatory processes or transient metabolic compromise, so diffusion-weighted imaging (DWI) had to be understood in clinical context.
However, in neonates, DWI findings may not match the severity of injury, the latter being lesser or greater than the imaging suggests. Grant urged caution because delayed cell death can evolve over time in children.
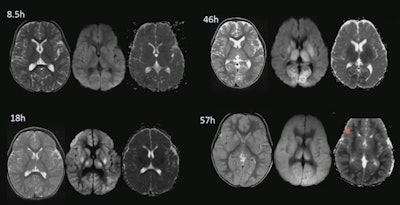 DWI and the ADC image shows a 2-year-old child who had choked on a candy. DWI and ADC images revealed only slight necrosis at 30 minutes after injury. However, the child was pronounced dead four days later, as the brain necrosed and swelled. Images show progress of delayed cell death
DWI and the ADC image shows a 2-year-old child who had choked on a candy. DWI and ADC images revealed only slight necrosis at 30 minutes after injury. However, the child was pronounced dead four days later, as the brain necrosed and swelled. Images show progress of delayed cell deathHyperperfusion confusion
With delayed cell death mind, areas of hyperperfusion in neonates should be looked at carefully. Hyperperfusion can be difficult to spot on MRI, but this can be helped by using arterial spin labeling (ASL), which provides more data.
With returned perfusion, injuries may continue to evolve. Imagers need to understand why there is high blood flow and the mechanisms triggering it.
Optical bedside devices such as frequency domain near infrared spectroscopy and diffuse correlation spectroscopy allow the measurement of cerebral blood flow and cerebral oxygen consumption and can indicate what is driving perfusion changes.
"When blood flow returns, you can have transient recovery of the energy metabolism and then go to delayed cell death," noted Grant. "When injuries increase over time, it isn't that necrosis has been missed, but it was because it wasn't there before."
Radiologists therefore need to understand these different types of cell death and the fact that the signature increased blood flow suggests an area that may undergo delayed cell death.
Q&A session
In the question-and-answer session, moderator Shawna Farquharson, PhD, SMRT 2019-2020 president, asked what development in MRI instrumentation has had the most impact -- hardware or techniques such as diffusion and perfusion imaging. The hardware and the newer techniques are intertwined, the one pushing the other, Grant noted, pointing to how 3-tesla scanning and phased-array coils also led to faster acquisitions, and very high-quality diffusion data.
SMRT president-elect Nancy Beluk passed on a message from the floor by asking to what extent ASL was used in newborns. Grant noted that ASL was helpful for determining flow, but it isn't quantitative in neonates and experts are still trying to optimize it for this population.
"It is useful for seeing whether there is a hyperperfusion response, for example in encephalopathic patients with subclinical seizures -- then this will be shown as high blood flow on ASL. However, further technical development is needed to develop ASL values in neonates," Grant said.