Mass casualty incidents (MCI) are rare, but preparedness and optimum use of CT are vital for any any medical imaging professional on the front line treating high casualty numbers with limited resources, international experts told attendees at a special session during ECR 2020.
Radiologists should be aware of how injuries from different types of weapons may present on CT scans, according to Dr. Elizabeth Dick, consultant radiologist at London's Imperial College NHS Trust. She drew attention to the principles of blast physics, in which the primary high-pressure blast wave will affect air-filled and fluid-filled structures such as the sinuses and bladder.
In the open air, severity of injury tails off quite rapidly at 2.5 meters from the blast center, while in closed spaces the blast wave will bounce around surfaces and be amplified, resulting in more severe injuries.
"A common finding is blast lung, a perihilar hazy shadowing which is a sign that the patient was close to the blast center," Dick noted.
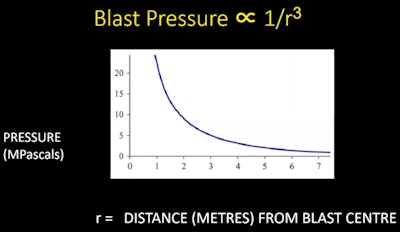 Table showing blast pressure in relation to distance from center of blast. All images courtesy of Dr. Elizabeth Dick, Imperial College NHS Trust.
Table showing blast pressure in relation to distance from center of blast. All images courtesy of Dr. Elizabeth Dick, Imperial College NHS Trust. In enclosed space, the blast wave bounces around and gets amplified, and these patients will have more severe injuries.
In enclosed space, the blast wave bounces around and gets amplified, and these patients will have more severe injuries.This type of radiological sign is a marker of severe injury, so if visualized, radiologists should be looking for injuries elsewhere. She noted that in such cases, CT may reveal perihilar ground-glass shadowing when x-rays may be normal.
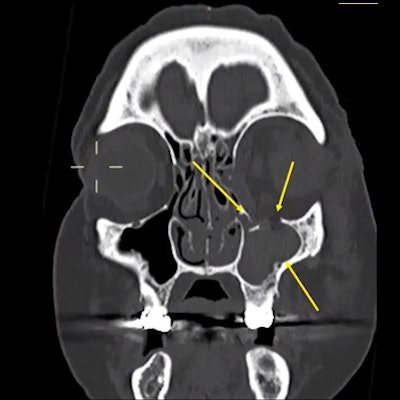
Although fractures and bleeding to other structures such as the maxillary sinus can be seen very clearly on CT, she urged imagers to consider a facial x-ray initially and perform the CT scan later as high patient numbers and CT demand after a mass casualty incident may be overwhelming.
"In each case offer abbreviated care and notes," she urged.
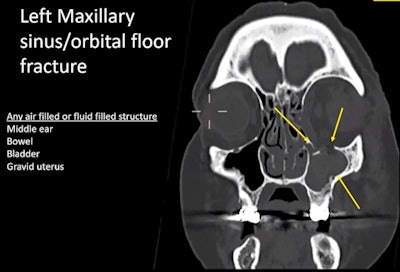 CT shows maxillary sinus fracture from blast and infilling of blood.
CT shows maxillary sinus fracture from blast and infilling of blood.Shrapnel visualization
Secondary blast injuries due to flying fragments such as glass, metal, and bone can be complex to locate and accurately interpret. While a CT scout view can provide a reliable overview of these potentially widely dispersed fragments within the body, such shrapnel does not have a linear trajectory and instead bounces around the body.
"Where they end up does not tell you where they have been, and that means we should have a low index of suspicion for suspecting another injury," noted Dick. "You should also consider a CT angiogram to check the vascular supply."
Pregnant women involved in mass casualty incidents should be given special consideration: Amniotic fluid will amplify the blast wave, and so baby and mother will be at increased risk of injury. Furthermore, keeping children together with their carers during treatment, including going to CT, will improve outcomes, according to Dick.
Gunshot wounds
ECR 2020 attendees also heard how in any firearm injury, the same principle applies: The bullet passes through the tissue, causing a permanent cavity; then around this, a temporary cavity is formed, where energy is also delivered. This can provide clues about injury extent.
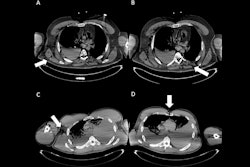
Dick demonstrated by showing two CT images, each depicting a different patient, both of whom had been shot in the chest with a different gun, and each with an anterior pneumothorax. In patient A, CT showed a relatively wide permanent cavity, indicating a higher-energy wound, and the bullet had passed out of the body. In patient B, the permanent cavity was narrower, and the bullet was still embedded posteriorly.
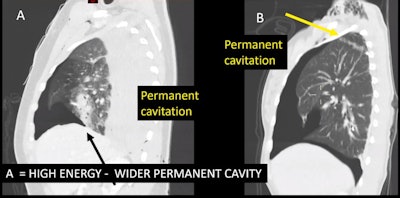 Patient A has high energy wound with wide cavity. In patient B, the cavity is narrower and the bullet is lodged posteriorly.
Patient A has high energy wound with wide cavity. In patient B, the cavity is narrower and the bullet is lodged posteriorly.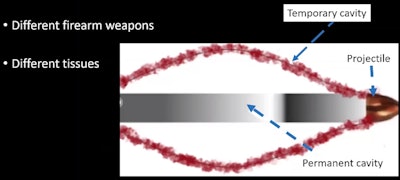 Gunshot wounds comprise a permanent and temporary cavity, regardless of firearm and tissue.
Gunshot wounds comprise a permanent and temporary cavity, regardless of firearm and tissue.If a bullet has already passed out of the body, radiologists will have difficulty discerning which wound is entry or exit. To avoid potential legal problems, doctors shouldn't try to second guess this in their reports.
Knife wounds
Providing eight top tips for knifings, Dick noted the following:
- Such wounds may be subtle -- if there is an underlying injury but no evident knife wound next to it, ask the clinician to check again.
- Contrast should be injected on the side opposite to an upper limb injury to avoid streak artifact from a vein obscuring an artery.
- Performing separate arterial and venous phases is essential.
- For neck injuries, think about the aerodigestive tract, which may be pushed over by hematoma.
- Consider the diaphragm even with small single wounds to the midabdomen, particularly if there is blood above and below the hemidiaphragm.
- Imagers should also check areas such as the retroperitoneum, the lesser sac, and the mesorectum. Surgeons tend not to check these areas unless the radiologist can guide them to injuries ahead of surgery.
- Abdominal injuries may have delayed presentation.
- Radiologists should have a low threshold for repeat imaging.
Disaster preparation
Activating a radiology plan for mass casualty incidents ahead of any mass influx of patients is an urgent priority, according to radiologist Dr. Marco Armbruster from Ludwig Maximilian University (LMU) of Munich, who discussed the best ways to prepare for the unpredictable in his presentation.
The key factor in any strategy is to identify potential bottlenecks in the system and formulate a clearly defined written plan, according to Armbruster, noting that LMU consolidated such a plan after a mass shooting incident in Munich in July 2016.
Besides the rapid mobilization of staff via various means including instant messaging applications, departments need a clear electronically registered patient identification method such as the barcode system, which not only helps to avoid order duplication but also can be used to archive scans. Further, as nonemergency imaging is canceled, scoring systems such as the Manchester trauma imaging score (ManTIS) will help define which MCI patients should be selected for whole-body CT scans.
Avoiding the pitfalls
A minimal accepted care approach aimed at preventing diagnostic bottlenecks in mass casualty incidents should also be defined in the plan, Armbruster noted.
This might involve scanning patients using focused assessment with sonography for trauma (FAST) and x-ray for spine, thorax, abdomen, and pelvis injuries (to diagnose pneumothorax or free intra-abdominal air or fluid, as well as unstable fractures), while CT is reserved for suspected severe head injuries.
For CT, a single-acquisition whole-body multidetector-row CT-scan with a rapid imaging protocol for trauma should be preferred over segmented whole-body CT. Such a rapid protocol might include a noncontrast CT of the brain, a CT angiogram of the vertex to pelvis, and a portal-venous CT of the abdomen and pelvis. Alternatively, radiologists may prefer to perform a CT angiogram and portal-venous phase in one single scan using a split bolus technique.
Data volume
The high volume of scans made in a short period of time during a mass casualty incident vastly increases the amount of data sent over the intranet, and this will potentially slow down the system, so simulation of high-volume scenarios to detect problems in advance is a vital part of preparedness. Furthermore, standard image reconstructions in different planes are time consuming and increase the number of images transferred to PACS, also causing delays.
"It might be preferable to transfer only 5-mm axial slice reconstructions in soft-tissue kernels during the surge. Additional reconstructions can be sent later or on demand from the reporting radiologist," Armbruster said.
Initial reporting straight after the scan should focus on life-threatening findings and be sent directly to the referring physician. Importantly, this report should use templates with checkboxes focusing on the relevant findings, and these reports should also serve as backup in case of PACS failure. A secondary survey and full report can be made later, he noted.
Mass casualty incident simulation and training should be regular events in any department, concluded Armbruster. This helps to estimate the surge capacity of each modality, identifies weak points in the protocol, flags potential PACS issues due to increased scan volume, and improves staff familiarity with their roles during an incident.