Failing to ensure patients receive appropriate intravenous (IV) access when they leave the emergency unit or hospital ward before a contrast-enhanced CT scan often results in significant waste of resources, a U.K. audit has found. The researchers have produced a five-point action plan to address the problem.
"Arriving for contrast-enhanced CT scans without appropriate IV access can result in delays in diagnosis and patient management, and may cause undue distress to the patient," noted Dr. Liisa Chang and colleagues from the radiology department at Kingston Hospital National Health Service (NHS) Foundation Trust, south-west London.
At RCR Digital 2020, the Royal College of Radiologists' (RCR) online learning program, they reported that the productivity of the radiology department falls for three main reasons:
- Direct CT scanner downtime. The lack of appropriate IV access is most commonly discovered once the patient is already on the gantry. Cannulating patients or repeatedly transferring the patient on and off the CT scanner leads to scanner downtime.
- Time required for radiology department staff to cannulate the patient in the CT scanner and for radiology staff to contact the clinical team/ward to organize appropriate IV access.
- Delays as a result of sending the patients back to the ward and organizing their return at a later time.
Ultimately, patients spend more time in the radiology department, which can have a negative impact on patient experience of care, they stated.
Data gathering
Chang and colleagues sought to quantify the time lost when patients are sent to the CT scanner from a ward or the accident and emergency (A&E) department without an appropriate, functioning IV access in situ.
Over a four-week period in November/December 2019, the authors examined CT scans carried out on 1,458 patients. Of these, 224 studies were excluded as outpatient/general practitioner studies. Of the remaining 1,234 scans classified as "inpatient" or "A&E," 424 were vetted as contrast-enhanced studies (424/1,234, 34%).
The authors collected the following information: date of examination, source of patient (the ward or A&E), whether IV contrast was specified at time of vetting, whether pre-CT instructions were sent to a ward, reasons for absent/inappropriate IV access, and outcome and estimated time to enact outcome. They performed retrospective analysis of the recorded cases with the Soliton radiology information system (RIS), focusing on the recorded radiographer notes/flags and any electronic time stamps.
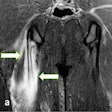
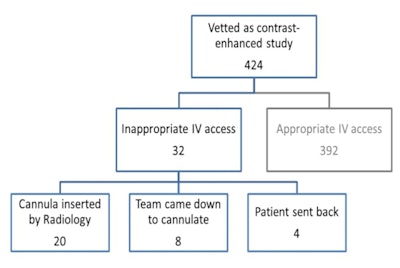 Outcomes in cases of absent or inappropriate intravenous access. In most cases, radiology staff inserted a cannula. All figures courtesy of Dr. Liisa Chang.
Outcomes in cases of absent or inappropriate intravenous access. In most cases, radiology staff inserted a cannula. All figures courtesy of Dr. Liisa Chang.Of the 424 patients, 32 (7.5%) arrived for imaging without appropriate IV access. In all 32 cases, pre-CT instructions confirming the need for appropriate IV access were communicated to the ward or A&E before the patient was transferred to the radiology department.
In most cases (20/32), a cannula was inserted by radiology in the department, and around 160 minutes were spent on this task. To put this into context, a standard appointment slot for inpatient and A&E CT examinations is 15 minutes, so 160 minutes translates to approximately 11 studies. A standard appointment slot for outpatient CT examinations is 10 minutes, meaning 160 minutes translates to 16 studies, they explained.
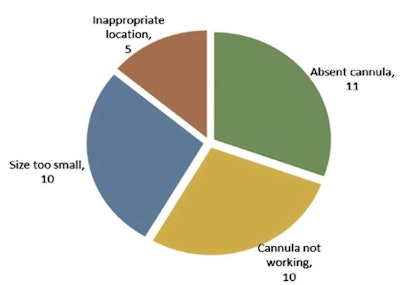 The rationale for inappropriate intravenous access (totals up to over 32, as multiple reasons were recorded for some patients).
The rationale for inappropriate intravenous access (totals up to over 32, as multiple reasons were recorded for some patients).The limitations of the study mean the audit underestimates the frequency of inappropriate IV access, as well the departmental productivity/time lost, the authors continued.
Prospective data collection relies on accurate recording of each incidence, and although attempts were made to raise awareness of the audit with a cohort of CT radiographers, a review of RIS revealed notes/flags for inappropriate IV access on studies not recorded on the data collection paperwork. This audit, therefore, only reports the number of cases of inappropriate IV access during our data collection period, they stated.
Secondly, not all responses were filled in correctly on the data collection sheet. Most problematic was "time patient spent in department," where several responses did not specify a numerical time value. Consequently, the estimated time lost is also a gross underestimate of the true CT scanner downtown and workforce time/productivity lost.
Future plan of action
Following analysis of the study, the Kingston team agreed on these measures and presented them to a departmental audit/governance meeting in January 2020:
- The vetting radiologist should remind the referrer about the need for appropriate IV access for contrast-enhanced CT scans at the time of the initial discussion.
- Updating local portering slips should include a tick box of "cannula present" for patients requiring contrast.
- The potential exists for implementing a pre-CT/pre-transfer checklist on the wards and A&E department for the entire hospital group. This should include assessment for functioning IV access; e.g., a specific request for a cannula to be flushed prior to patient transfer to the radiology department.
- Dissemination of results to the wards and A&E department, accompanied by another audit.
- Further increase awareness of the audit with the cohort of CT radiographers prior to prospective data collection, and with interval reminders to ensure a more complete data collection.
Plans for a second audit to monitor the success of the approach have had to be delayed due to the COVID-19 pandemic, Chang and colleagues concluded.