The quality of prostate MRI images influences the accuracy of image-based diagnostic decisions, and compliance with PI-RADS recommendations is not the only important factor influencing the image quality, a new Dutch study has found.
In a study published on 5 April by Insights into Imaging, Dr. Linda Thijssen of Radboud University Medical Center in Nijmegen, the Netherlands, and colleagues sought to establish current compliance with PI-RADSv2.1 recommendations and identify other factors possibly influencing MRI quality.
The researchers used a survey sent to Dutch medical centers to determine how MRIs were performed, as well as compliance with PI-RADS recommendations. In addition, they conducted a reader study on prostate MRIs submitted by respondents to evaluate the image quality. They also assessed any associations between image quality and factors including personnel education, patient preparation, MRI hardware used, and technical parameters.
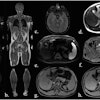
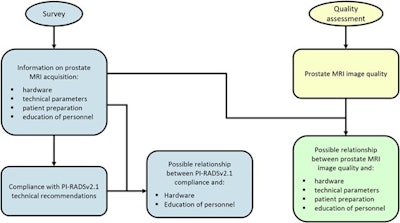 Infographic on study organization. Blue: section of the study based on the survey. Yellow: section of the study based on the reader study. Green: section of the study based on both survey and reader study. Figure courtesy of Dr. Linda Thijssen et al. and Insights into Imaging.
Infographic on study organization. Blue: section of the study based on the survey. Yellow: section of the study based on the reader study. Green: section of the study based on both survey and reader study. Figure courtesy of Dr. Linda Thijssen et al. and Insights into Imaging.
Of the 68 medical centers the study team sent the survey to, 44 submitted only their compliance with PI-RADSv2.1 technical recommendations, while 26 completed the full survey. Thirteen hospitals provided 252 usable images from anonymized prostate MRI examinations of biopsy-naive men suspected of prostate cancer. The mean compliance with PI-RADS recommendations was 79%.
The results from the survey showed that while compliance with PI-RADS recommendations was high, 30% to 50% of the prostate MRI examinations were of inadequate image quality.
Among the factors potentially associated with image quality, specialized education for the radiologist was significant. The findings showed that images from hospitals where radiologists had taken a dedicated course on reporting prostate MRI received higher quality scores, in particular on T2-weighted (T2W) signal-to-noise ratio (SNR), total T2W quality, and total biparametric quality.
“Prostate MRI educational courses should not solely focus on interpretation, but cover quality assessment as well, and include knowledge of potential causative factors to enable radiologist to adapt their protocols to obtain improved image quality,” the authors stated, while also noting that recent studies have shown that courses on assessing prostate MRI quality also improve application of the PI-QUALv1 scoring system.
Interestingly, they found no correlation between the center’s compliance with PI-RADS recommendations and attendance of a dedicated prostate MRI course by a radiologist.
Patient preparation, which included steps to reduce image degradation and motion artifacts -- such as the use of an antispasmodic agent to prevent bowel movement or a rectal catheter to evacuate gas to reduce image degradation -- had a positive influence as well. However, the researchers said that these steps were sometimes used sporadically.
The researchers also noted positive correlations with image quality and hardware used; the positive effect of higher field strength on image quality has been remarked upon in other studies, they said, and it can be explained by the higher SNR, for example.
Regarding the PI-RADS scoring, the authors offered a caution, pointing out that some of the technical recommendations seemed to have a negative influence on image quality -- such as interslice gap and small field-of-view -- when the parameters are “nearly compliant” with the recommended value.
“[T]he PI-RADSv2.1 technical recommendations are meant to achieve adequate coverage and detailed images of the prostate, not to optimize image quality,” the authors wrote.
The authors noted limitations of their study: they suggested that it was possible that only hospitals that were confident in the quality of their images chose to submit images for quality assessment, which may have led to an overestimation of the image quality. They also stated that factors other than those they examined may have affected image quality as well; these additional factors could be explored in future research, they added.
Read the article here.