A major challenge facing breast radiologists in sub-Saharan Africa is that women often present when cancers are advanced. More patient education and support and a stronger primary healthcare system are vital to allow for timely diagnostic referrals, according to new research from Tanzania.
In Tanzania, the number of new cases of all types of cancer doubled between 2006 and 2013. Half of those diagnosed with breast cancer will die of the disease, and an 80% rise in the number of new breast cancers and breast cancer deaths is expected by 2030.
The incidence of breast cancer is steadily growing due to increased life expectancy, increased urbanization, and adoption of Western lifestyles, and breast cancer is the second most common cancer and the second most common cause of cancer death among Tanzanian women. Breast cancer mortality rates are among the highest globally.
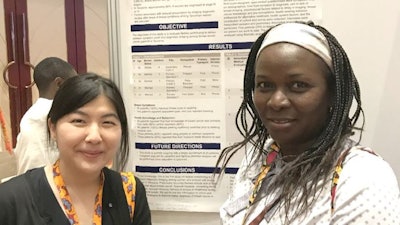 Dr. Lulu Sakafu and coauthor Dr. Amie Lee from UCSF. Photo courtesy of Dr. Lulu Sakafu.
Dr. Lulu Sakafu and coauthor Dr. Amie Lee from UCSF. Photo courtesy of Dr. Lulu Sakafu."Most patients (>80%) with breast cancers are diagnosed at stage III or IV. Large palpable lumps and bulky adenopathy is the usual presentation, and about 30% have distant metastasis at initial presentation," noted Dr. Lulu Sakafu, a radiologist at Muhimbili National Hospital (MNH) Mloganzila in Dar es Salaam, and colleagues in an RSNA 2020 e-poster for which they received a certificate of merit.
"Studies have shown delays of more than three months upon symptom onset leads to poor prognosis. Delays from symptom onset to presentation are often far longer in Tanzanian women," they explained.
Mammography screening in the public health system is not available, and this screening cannot be widely implemented until processes are in a place to better address symptomatic disease, they added.
Meeting the need for data
The radiology department at MNH Mloganzila is equipped with a mobile digital mammography machine and more than 12 ultrasound units. Dedicated radiographers and radiologists perform breast imaging and can carry out ultrasound-guided fine-needle aspiration biopsies and core-needle biopsies, and they work in close collaboration with pathologists, surgeons, and oncologists.
Sakafu and colleagues recently undertook a study to evaluate factors contributing to delays between symptom onset and diagnostic presentation. They recruited 12 women with pathologically confirmed breast cancer. In-depth, semistructured interviews from an open-ended questionnaire were conducted in Swahili, transcribed, and translated into English.
The researchers collected data on demographics, use or nonuse of breast imaging, psychosocial factors related to delay in imaging, breast cancer knowledge and preconceptions, health-seeking behavior, and the contribution of culture and norms. They performed qualitative analysis using Dedoose, a cloud-based coding application software.
The mean age was 50 years (range, 41-65). Five participants were educated to primary school level, five to secondary school level, one to college level, and one had no formal education. The most common occupations were "petty trader" and "peasant" (25% each). All women said their first symptom was self-identifying or a swelling. Two women had associated pain, and one woman had a discharge of blood.
Barriers to seeking medical help
Lack of cancer knowledge and financial worries among the participants were common barriers to seeking an early diagnostic evaluation.
"All participants admitted to recognizing a new breast symptom, but most didn't understand that it could be something serious like a cancer," Sakafu said. "Many were not worried and decided to ignore it. Most participants noticed a lump but decided to seek healthcare several months to more than a year later, after which symptoms had progressed to more severe stages."
Women said they struggled to get money to access healthcare, and this contributed to significant delays. Several women had to ask family members for funds, and after getting a referral to go for an imaging exam in a referral/national hospital, some had to decline due to lack of funds. Lack of awareness of imaging among healthcare providers at the primary level was another problem.
"Some participants believed that the disease was because they are being bewitched and hence have to be treated by a witch doctor," noted Sakafu, adding that women tend to be treated by witch doctors for more than three months before they realize they're getting worse, and only then do they go to the hospital.
Societal stigmatization of cancer led to some participants not speaking about their symptoms and holding back on seeking medical care. Some reported fears of others finding out.
"Poor cancer outcomes have instilled fear that it is an incurable disease or that going to the hospital is a death sentence," she said. "People feel it's a terrible disease that they must hide from others."
Family and friends can have a significant influence as both facilitators and barriers to care, and they sometimes allow participants to watch and wait rather than seek prompt medical attention. They also relate fears of the hospital to the participant, equating possible cancer diagnosis and treatment with death.
In some cases, other health conditions led participants to wait before seeking care for the breast cancer. Another factor was family responsibilities, with patients prioritizing attending funerals or taking care of sick relatives before taking care of themselves.
What are the solutions?
According to the authors, "Education on early recognition of signs and symptoms of breast cancer can empower women to seek early medical attention. Women can be targeted through social media campaigns, radio, or television. Breast health awareness education should be offered at local health centers."
Strengthening primary care and local healthcare providers is critical for an early diagnosis, they continued. Improving the capacity of primary care and the first point of contact in the health system can lead to a more timely diagnosis, they pointed out.
 Better staff training can help improve patient outcome in developing nations. Photo courtesy of UCSF Global Cancer Program.
Better staff training can help improve patient outcome in developing nations. Photo courtesy of UCSF Global Cancer Program.Diagnosis requires an efficient clinical evaluation, referral process, and timely coordination of services that include proper evaluation upon initial presentation of a breast complaint, a trained workforce starting with primary care providers, clinical breast exams performed by primary care providers, no breast ultrasound scans by untrained sonographers, and a timely and clear referral system.
At referral hospitals, advanced services, including imaging, need to be available. Breast ultrasound, tissue sampling (e.g., ultrasound-guided biopsy), tumor-node-metastasis (TNM) staging, more mammography and ultrasound machines, a national strategy and approach, and routine determination of TNM staging through imaging are all necessary, they said.
Support from overseas
Sakafu's study, entitled "Evaluation of Factors Related to Delay in Imaging Presentation of Women with Breast Cancer in Tanzania," was granted UCSF-MUHAS Cancer Collaboration Pilot Award funding. Co-investigators included Dr. Flora Lwakatare (head of radiology at MNH) and Dr. Lulu Fundikira (head of radiology at Muhimbili University of Health and Allied Sciences, MUHAS). Dr. Amie Lee, assistant professor of radiology at University of California, San Francisco (UCSF) served as a co-investigator and research mentor.
In August 2018, seven faculty members from Ocean Road Cancer Institute (ORCI, the national referral center for cancer care in Tanzania) and MUHAS, including Sakafu, went to UCSF for a five-week clinical-research training course.