How can virtual reality (VR) and augmented reality (AR) help radiologists advance their specialty's value in healthcare? Researchers from the Netherlands, Sweden, and the U.K. drew from their experiences with the technologies to discuss the possibilities in a Thursday Coffee and Talk session at ECR 2019.
In recent years, clinicians have begun exploring potential medical applications for VR and AR, including for resident training, patient education, and intraoperative guidance. Much of the actual handling of these technologies has been managed by physicians other than radiologists.
So why should radiologists bother when they already have their computer screens? That was a key question Peter van Ooijen, PhD, a computer scientist at the University of Groningen in the Netherlands, asked in his opening talk.
One of the most important aspects of VR and AR is acquiring the proper imaging data. "You need a good quality image without too much noise and with correct segmentations of the data. ... The role of radiology [in this process] is really large," he said.
To make the case, Dr. Anders Persson, PhD, from Linköping University in Sweden, explained how radiologists and 3D imaging specialists at the university's Center for Medical Image Science and Visualization play a pivotal role in supplying imaging data for their 3D virtual models. These data provide the framework for educating medical students, residents, and patients using VR and AR headsets.
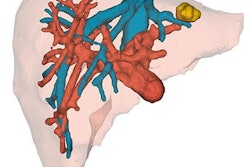
With AR, for example, multiple users can examine a patient-specific 3D anatomical model at the same time, allowing them to see inside the patient and grasp the true depth of cardiac anatomy, Persson said.
Surgeons, too, have been taking advantage of the advanced visualization and high mobility afforded by AR technology. Traditionally, radiologists prepare a textual report of medical images for surgeons to read as they prepare for procedures. But surgeons generally do not have the means to access a considerable portion of the information contained within the reports during an operation, Dr. Dimitri Amiras of Imperial College Healthcare National Health Service (NHS) Trust in the U.K. noted in his talk.
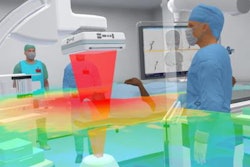
AR technology enables radiologists to provide surgeons with critical imaging information as they perform a procedure, he explained.
At their hospital, for instance, Amiras and colleagues have used AR to facilitate plastic reconstructive surgery. In one case, radiologists segmented the imaging data of a patient scheduled to undergo reconstructive leg surgery and then converted the data into 3D models compatible with AR software. They emphasized highlighting the vascular anatomy of the patient during image segmentation so that the surgical team could safely perform the procedure without perforating any veins or arteries.
For radiologists preparing AR models, "the most important step is image segmentation," Amiras said. "This allows the radiologist to effectively tell the surgeon, 'This is the important data. I've interpreted this image, and I'm telling you where you need to do the surgery.' Without the right information segmented, the surgeon could operate on the wrong vessel."
"I really think this is going to be a game-changer for surgery," he added. "And using this technique, we will not only be able to make things quicker and faster, we may start to make the inoperable operable. I think this is the future."