Few people have had greater individual impact on the evolution of CT scanners than Dr. Willi Kalender, PhD, the pioneer of spiral systems. As the director of the Institute of Medical Physics at the Friedrich-Alexander University of Erlangen-Nürnberg in Germany, he is currently overseeing projects relating to CT imaging of the heart, micro-CT, and image-based navigated interventions.
Patient dose estimates represent a dilemma. Even though there has been a significant amount of research regarding patient dose assessment, international consensus has not yet been reached and further improvements are needed, according to Kalender.
Patient dose estimates from CT examinations are based primarily on Monte Carlo (MC) calculations using anthropomorphic phantoms. Direct measurements are neither practical nor do they allow for the assessment of the spatial distribution of dose. Today's CT dose index (CTDI) concepts are excellent for scanner characterization, and acceptance/consistency testing, dose estimates are based on standard CTDI phantoms, but they do not take into account the specifics of a patient's individual body habitus and do not provide patient dose or organ dose values.
Size-specific dose estimates (SSDE) have been proposed by a task group of the American Association of Physicists in Medicine (AAPM), but in Kalender's opinion, further consensus decisions and methods to determine patient diameters are needed to achieve a general acceptance of this concept. Calculating an effective dose can be valuable for comparison of technologies and specific patient population groups, but its limitations do not make it an appropriate measure for individual patients.
Kalender has proposed a different approach to patient- and organ-specific dose estimates (POSDE). Patient CT data are used to provide comprehensive information about a patient's body shape in the region that was scanned. The data are appended at the top and bottom of the available image volume by data taken from size-adapted anthropomorphic voxel phantoms. The result is a patient-specific whole-body voxel phantom suitable for MC dose calculations that provides definitions of organs inside and outside the scanned range. Reliable scanner- and scan protocol-specific information is then obtained, but this estimation is limited to dose for organs that are clearly delineated and does not include skin, mucosa, or bone marrow.
Like SSDE, the POSDE approach is still a work-in-progress. Kalender believes radiologists need to realize that while organ doses can be estimated with high accuracy, this process is complex and time-consuming. It should be limited only to patients for whom this knowledge can have impact on patient management with respect to imaging.
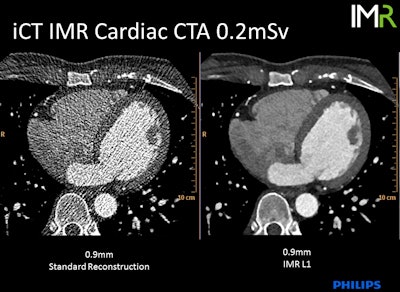 0.2-mSV cardiac CT angiography examination demonstrates standard reconstruction versus iterative model reconstruction (IMR). Image courtesy of Philips Healthcare.
0.2-mSV cardiac CT angiography examination demonstrates standard reconstruction versus iterative model reconstruction (IMR). Image courtesy of Philips Healthcare.Dose-reduction strategies
Understanding the principles of radiation protection and imaging procedures is an essential prerequisite for candidates preparing for the European Diploma in Radiology (EDiR) examination and also radiologists in practice. Today's EuroSafe session presented by three expert medical physicists provided an overview of CT, MRI, and radiation protection.
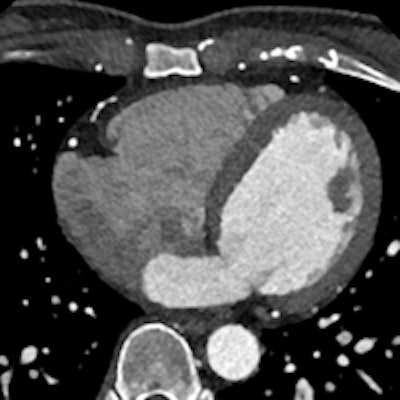
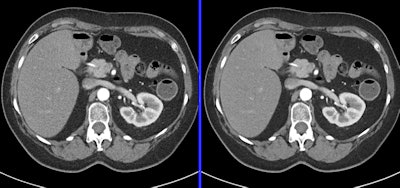
 Dose-monitoring software such as DoseWatch can automatically evaluate the size-specific dose estimate (SSDE) following the American Association of Physicists in Medicine's (AAPM) Task Group Report 204 version. The SSDE is a metric developed by the AAPM to evaluate dose according to patient size. Image courtesy of GE Healthcare.
Dose-monitoring software such as DoseWatch can automatically evaluate the size-specific dose estimate (SSDE) following the American Association of Physicists in Medicine's (AAPM) Task Group Report 204 version. The SSDE is a metric developed by the AAPM to evaluate dose according to patient size. Image courtesy of GE Healthcare."The use of imaging is growing globally. It is imperative that radiology trainees recognize that more CT imaging procedures will be performed in the generations of patients they will be treating as compared to mid- and advanced career radiologists," stated Mahadevappa Mahesh, PhD, chief medical physicist at Johns Hopkins Hospital in Baltimore, Maryland, U.S. "Radiation protection is of paramount importance for both patients and professionals performing imaging. New radiologists need to be proactive about this and maintain diligence about reducing radiation dose whenever possible without jeopardizing image quality.
Radiology trainees need to be champions of radiology department culture to monitor image quality and examination dose. They should be willing to request review "outlier" examinations they have performed or interpreted with lead radiologists of the department or imaging section. Outlier exams are ones that either have a higher than expected dose or have poor image quality for the indication, which may suggest the use of overly aggressive dose-reduction strategies.
"The primary goal with dose-reduction efforts is to preserve the diagnostic performance of CT. This in turn, is influenced by the image quality. For this reason, indication-based image quality delivery is the most desirable approach," he added.
Mahesh said that maintaining image quality is critical for protocols involving liver or pancreas CT scans, for example. By comparison, CT angiograms, CT colonoscopy, and CT enterography can use protocols with slightly lower image quality.
Mahesh noted that current scanners are complicated, and protocols should be tailored to specific patient size, anatomy imaged, and clinical indications for the exam. He offered these practical steps to update and modify CT protocols with the goal of dose reduction:
Adopt manufacturer-specific CT protocols developed by subspecialty societies, such as the AAPM, and organizations dedicated to dose reduction, including Image Gently and Image Wisely.
Tailor protocols to the clinical indication.
Review protocols examining section collimation and be creative. It is possible, for example, to reconstruct thinner coronal and sagittal reconstructions from volumetric/isotropic CT data to complement thicker axial images.
Use tube current modulation software that has the ability to lower dose by as much as 40%.
Use tube current overrides when a patient is not average-sized.
Vary tube voltage based on patient size and the examination indication, using patient weight, diameter, and/or body widths as guides for selecting tube voltage values.
Ensure that patients are correctly positioned in the isocenter of a CT scanner. If a patient is placed closer to the tube rather than in isocenter, the scout image will appear to be larger and the automatic tube current modulation will mistakenly create settings for a larger-bodied patient.
Limit phase and image creep.
Use iterative reconstruction algorithm software if it is available.
Establish a dedicated CT protocol team to regularly monitor protocols and techniques to further reduce dose. Maintaining image quality and patient safety is an ongoing process.
These two overviews on CT dose provide excellent primers for both radiology trainees and experienced radiologists:
- Kalender WA. Dose in x-ray computed tomography. Phys Med Biol. 2014;59(3):R129-R150.
- Mayo-Smith WW, Hara AK, Mahesh M, Sahani DV, Pavlicek W. How I Do It: Managing Radiation Dose in CT. Radiology. 2014;273(3):657-672.
Originally published in ECR Today on 8 March 2015.
Copyright © 2015 European Society of Radiology