Despite severe reimbursement cuts, limited healthcare spending and the threat of European legislation, MRI remains one of the leading diagnostic imaging modalities. It has also become the new champion of radiology for general imaging, picking up the slack following the dose concerns and misuse of CT.
In recent years, development of application-focused MRI technology has appeared to slow. Improvements on scan speed, workflow, and operating cost are welcome developments, broadening the availability of MR imaging during austere times. Few of these developments, however, have offered new insight for clinical diagnosis -- but that might be about to change. Could MRI finally be on a path toward greater clinical specificity?
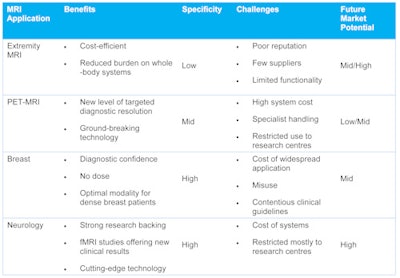
Extremity MRI: Overlooked and undervalued
Extremity MRI has long been seen as a secondary market for cash-rich specialist orthopedic clinics. Yet as healthcare providers search for more efficient, cost-saving solutions, the relevance of extremity MRI has increased. Improvements in extremity MRI technology have also helped raise interest, offering an intriguing alternative MRI workflow. It is common knowledge that central hospital MRI systems are often overbooked, with patient waiting time for MRI scans often months long. What is less well-known is the proportion of extremity MRI scans performed on whole-body scanners. Recent estimates suggest it could be as high as one-quarter. Yet extremity systems accounted for approximately 7% of the global revenue total last year. Surely utilization of the newest generation of extremity MRI systems as "overflow" units for busy hospital MRI systems makes clinical and financial sense for many users.
Nonstandard MRI: Expanding diagnostic horizons
Some of the most effective advances in imaging recently have not necessarily been purely due to MRI technology advances. Instead, collaboration with other modalities has led to innovative new diagnostic techniques. Fusion imaging, using MRI and ultrasound or interventional x-ray has been particularly prominent, mostly due to the efficiency and improvement in guidance offered with dual-modality imaging. PET/CT imaging has also become far more regularly used, especially in oncology and radiotherapy planning. PET/MRI is also close to commercial availability; despite the eye-watering costs, it is touted as the next major advance in diagnostic imaging. However, IT is offering a far cheaper solution in the meantime. Overlaying and fusing PET/CT images with high-resolution MR imaging could provide a far less expensive "virtual PET/MR" solution, or until real PET/MR becomes more affordable and available. Watch this space.
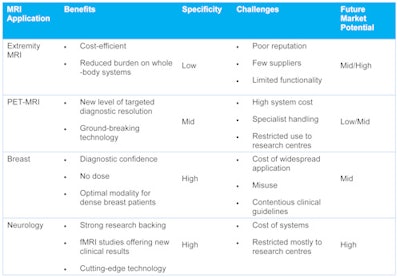
Breast MRI: Misguided but still a role to play
Breast MRI is currently one of the most heated debate topics among healthcare providers. Realization that breast screening and diagnostic pathways should be more patient-specific has also raised the profile of MRI as an alternative to conventional mammography. Breast density remains at the core of the issue, with support for adaptive diagnostic pathways based on patient breast density growing day by day. High-profile legislation legally requiring physicians to tell patients their breast density also has fueled the debate.
Expanding the scope and regularity of MRI use is a positive development for the MRI market, with vendors keen to capitalize on the high-profile and contentious topic of breast screening. However, to date, the application of breast MRI has been relatively misguided and patchy. Clearly, the future for breast MRI should form part of a diagnosis pathway based on breast density. Use should be limited to patients who have already had mammography or 3D tomosynthesis scans, or automated breast ultrasound scans. Only if both are inconclusive should MRI be used due to the high cost and significant demand on MRI resources. The same should also apply for procedural and diagnostic use; it should be used as a last resort if ultrasound or initial scans need additional clarification. This has also been highlighted by recent research on the overuse of MRI for preoperative breast surgery in low-risk cases, where MRI use is shown to offer little clinical benefit to care. This may change moving forward as reimbursement for MRI continues to decline. However, in order for MRI to be used most effectively, the ongoing debate into breast screening needs to lead to a formal, universal, adaptive care pathway. Only then will MRI be most effectively used to offer a patient-focused solution.
Neurology: At the cutting edge
Neurology is currently experiencing a wave of interest, spurred by high-profile government policies and vendor focus on neurology-specific MRI tools. The recent realization that 7-tesla MRI could be viable in the future for more widespread research also has spurred on development in this field. Admittedly, the majority of advancements have been at the premium end of the market, especially highlighted by intriguing partnership of functional MRI and the emergence of fully integrated PET/MRI. With rising awareness of neurological conditions such as Alzheimer's and schizophrenia, development of neurology-specific MRI technology will surely continue. This could also mean neurology-specific tools will become more widely available in less expensive systems, prompting the possibility of widespread MRI screening for neurological disorders in the not too distant future.
Stephen Holloway is the associate director of medical devices and healthcare IT research at IHS. He can be reached at [email protected].
The comments and observations expressed herein do not necessarily reflect the opinions of AuntMinnieEurope.com, nor should they be construed as an endorsement or admonishment of any particular vendor, analyst, industry consultant, or consulting group.
Originally published in ECR Today on 7 March 2014.
Copyright © 2014 European Society of Radiology



















