VIENNA - Multidisciplinary team meetings are coming for you -- or at least you can expect them to be more common in the future, according to Italian researchers. In a Saturday session, a radiologist, surgeon, pathologist, and others came together to answer questions about what it's like to work as a team and to explain why they think multidisciplinary team meetings are the wave of the future.
In an interview with ECR Today, the researchers from Milan said considering the clinical and even the medicolegal climate, they think multidisciplinary team meetings will definitely become more commonplace, and probably of "crucial importance" in patient management.
Their session, "Multidisciplinary team meeting from Milan, Italy," offered a perspective on what it's like to work within a multidisciplinary model specifically for breast imaging. All of the researchers hail from different departments -- Dr. Pietro Panizza comes from the radiology department at the San Raffaele Scientific Institute, as does radiology resident Dr. Sara Viganó; Dr. Roberto Agresti and Dr. Laura Lozza come from the Instituto Nazionale dei Tumori, along with Drs. Biagio Paolini (pathology department) and Giulia Bianchi (oncology department) at the same institution -- but they work together to treat breast cancer patients.
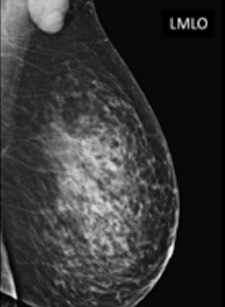
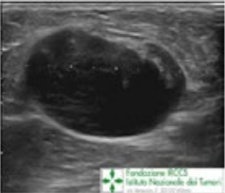 A 65-year-old patient presented with a recent history of a new lump in the left axilla. Clinical examination confirmed a discrete hard palpable mass in the left axilla, in keeping with suspicious finding without clinical breast abnormalities. Mammography and ultrasound were required. Corresponding to the palpable lump, on left mammogram (top) is a rounded mass without any breast lesions, and on ultrasound (bottom) a hypoechoic lesion with no hilum, in keeping with malignant metastatic lymph node. All images courtesy of Dr. Pietro Panizza.
A 65-year-old patient presented with a recent history of a new lump in the left axilla. Clinical examination confirmed a discrete hard palpable mass in the left axilla, in keeping with suspicious finding without clinical breast abnormalities. Mammography and ultrasound were required. Corresponding to the palpable lump, on left mammogram (top) is a rounded mass without any breast lesions, and on ultrasound (bottom) a hypoechoic lesion with no hilum, in keeping with malignant metastatic lymph node. All images courtesy of Dr. Pietro Panizza.
Their multidisciplinary team has to provide all the services related to breast cancer, including genetics and prevention, treatment of the primary tumor, care of advanced disease, palliation, and follow-up of previously treated women. The breast unit is made up of a group of dedicated breast cancer specialists, including a radiologist, radiographer, surgeon, reconstructive surgeon, pathologist, medical oncologist, radiation oncologist, and breast care nurse.
The specialists involved in breast cancer units have access to all the facilities required for high-quality care and spend most of their working time dealing with breast cancer. They organize weekly meetings to evaluate and plan patient care at any step of the diagnostic and therapeutic process. Each year, they treat about 1,500 newly diagnosed patients with primary breast cancer and about 10,000 patients in follow-up.
According to the researchers, the necessity of a multidisciplinary consensus in decision-making has always been perceived by clinicians, even in the past. As an example, in breast care, the importance of a general consensus on treatment decision and cooperation was strongly perceived when conservative treatment has been introduced. This is now an established standard of care, but it wouldn't have been possible without the support of team work, they noted.
Multidisciplinary work has become important not only in breast imaging but also in all radiology subspecialties. For instance, cancer treatment has become more complex, requiring a wide range of different expertise and including "noncancer issues" with a growing number of specialists and health professionals involved. As a consequence, a multidisciplinary organized approach cannot be disregarded any more. In fact, the European Partnership Action Against Cancer (EPAAC) consensus group stated: "Multidisciplinary teams emerge as a practical necessity for optimal coordination among health professionals and for clear communication with patients."
In the face of this increasingly complex care scenario, radiologists -- whatever subspecialty they are involved in -- cannot ignore the necessity of multidisciplinary team work any longer, the researchers insisted.
"It's not just about 'breast patients'; it's about every patient in order to deliver high-quality care throughout the care pathway and shift toward a patient-centered approach," they said.
How multidisciplinary teams are different
Functioning as a team affects an individual's workload and patient management. Coordination of different health professionals involved in patient care may improve patients' short- and long-term outcomes by influencing various aspects of care, for instance, primary breast surgery, management of the axilla, whether and when patients should receive chemotherapy and/or radiotherapy, and which kind, the researchers said.
A multidisciplinary approach can also do the following:
- Deliver a level of care that conforms to agreed standards and reflects national guidelines
- Allow better adherence to evidence-based decisions
- Create more coordinated patient care that can improve clinical decisions
- Result in a better planning of the care pathway concerning primary and reconstructive surgery, chemotherapy, radiotherapy, and radiological assessments
- Nurture shared decisions on clinical approved approaches, as well as get a consensus on newly innovative techniques or treatments
- Define and coordinate follow-up strategies (i.e., postoperative, along with neoadjuvant chemotherapy, or for patients not surgically treated)
- Boost time management due to cooperation and clearly defined pathways and guidelines
- Improve patient involvement in treatment decisions
- Help in problem-solving about organization and patient management
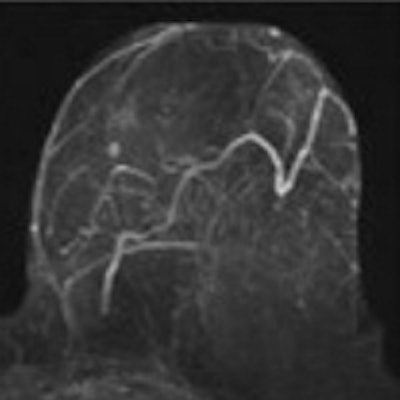
 Same patient as above. A second-look ultrasound was performed demonstrating an ill-defined, irregular lesion corresponding to the enhancing lesion on MRI. It was biopsied. At histology, it was an invasive ductal carcinoma, and the patient underwent conservative surgery. Chemotherapy was discussed and agreed upon in the multidisciplinary meeting.
Same patient as above. A second-look ultrasound was performed demonstrating an ill-defined, irregular lesion corresponding to the enhancing lesion on MRI. It was biopsied. At histology, it was an invasive ductal carcinoma, and the patient underwent conservative surgery. Chemotherapy was discussed and agreed upon in the multidisciplinary meeting."As radiologists, working in a multidisciplinary team leads to a better comprehension of the whole treatment strategy; we can for example, compare imaging with pathological results and discordant cases can be easily identified and opportunely/conveniently followed-up," they said. "We can be more involved in the care pathway not only as a diagnostic service, but also in the follow-up of neoadjuvant therapy, establishing together with clinicians the best imaging technique for every patient."
On the flip side, because the radiologist knows which therapy or treatment the patient has received, he or she can achieve a better interpretation of the imaging findings.
Centered image (change width in div style tag as needed)Nonetheless, working in a multidisciplinary team is not always straightforward. It requires cooperation and comparing different point of views that can lead to "complex and straggling discussions," they added. Also, the involvement of different disciplines, and even different clinicians within the same discipline, implies different perspectives and interpretations that can diverge and should be taken into account.
Working together as a team requires the capability to come face to face with "our own limits and accept others' advice, not as a critique on its own," but as possible constructive criticism. Moreover, organizing the whole multidisciplinary work may require a huge amount of time; everyone involved should shift from an individual way of thought to a shared one, which can't be taken for granted, they added.
All things considered, working as a team may make everyone more reassured with regard to patient management, because there is cooperation, strategy sharing, and coordination. Clinicians can boost their confidence in decision-making as the decision is strengthened by a general consensus.
"Improvements in the 'breast multidisciplinary model' are required as it's still a work-in-progress, but we hope that our experience might be a useful look through the benefit and the criticisms involved in multidisciplinary team work," the researchers concluded.
Originally published in ECR Today on 8 March 2014.
Copyright © 2014 European Society of Radiology



















