VIENNA - Trying to be more selective about which patients receive a CT scan following minor head injury (MHI) may sound like a good idea, but most of the major selective strategies are less cost-effective and riskier to patients than just routinely scanning all such patients. That's according to new data presented Friday at the 2008 European Congress of Radiology (ECR).
CT scans are used routinely regardless of cost for timely diagnosis of neurocranial complications in patients presenting with MHI. But the cost of such routine scanning has prompted clinicians and public health advocates to try to find ways to be more selective about who gets scanned.
"Given the low frequency of the complications and high number of MHI patients, it seems inefficient to scan all MHI patients," said Dr. Marion Smits from the Erasmus University Medical Center in Rotterdam, Netherlands.
However, her study comparing the cost-effectiveness of routinely scanning all MHI patients with CT versus using three different selective protocols -- plus no scanning, as a hypothetical reference strategy -- revealed that the sensitivity of several major selective protocols is currently too low to warrant their use in the clinical setting.
If a prediction rule is less than 97% sensitive in identifying MHI patients requiring neurosurgery, the selective method is not only less cost-effective than routine scanning but also risks compromising patient outcomes significantly.
"While the risk of selective strategies failing to find urgent cases for a CT scan is small, the consequences in terms of quality of life, or even loss of life, may be substantial and even outweigh the costs saved," Smits said.
The three selective strategies evaluated in the study were the Canadian CT Head Rule (CCHR, Lancet, May 5, 2001, Vol. 357: 9266, pp. 1391-1396), the New Orleans Criteria (NOC, New England Journal of Medicine, July 13, 2000, Vol. 43:2, pp. 100-105), and the CT in Head Injury Patients (CHIP) rule (Annals of Internal Medicine, March 20, 2007, Vol. 146:6, pp. 397-405).
The researchers used a decision tree and the Markov model, respectively, for determining short- and long-term cost-effectiveness. Key outcome measures were first-year and lifetime costs, quality adjusted life years (QALYs), and incremental cost-effectiveness ratio (ICER).
Each of the three strategies has in the past reported 100% sensitivity in identifying patients in need of a CT scan/neurosurgery. Based on the results of her study, however, Smits said that "we cannot assume that any of the currently published prediction rules are more than 97% sensitive to identify patients requiring neurosurgical intervention, since reported 95% confidence intervals for this sensitivity range as low as 85%."
 |
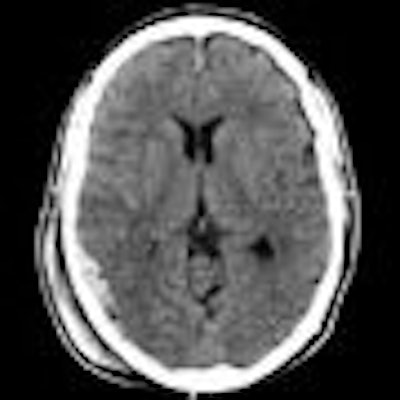
| Routine CT scanning may still be the best option for patients with minor head injury. Image courtesy of Dr. Marion Smits. |
Of the base-case analysis, comprising 10,000 41-year-old men, first-year costs were highest (35,437 euros or $54,375 U.S.) for MHI patients requiring an initial CT scan followed by surgery, but when no action was taken. This hypothetical strategy also gave the lowest efficacy, survival, and worst quality of life outcomes. Given the 95% confidence intervals in the study, there is a small but notable likelihood that selective strategies could produce this result.
The Canadian strategy (CCHR) was the least costly (6,941 euros or $10,648), proving also to be the most cost-effective overall of the selective protocols tested. The CHIP rule was more expensive but just marginally more effective. Of the three, the NOC system was shown to be the least cost-effective.
On the basis that these selective prediction rules cannot yet be relied upon to deliver more than 97% sensitivity, the research concluded that with an ICER of less than 60,000 euros ($92,068) referring all MHI patients routinely for a CT scan remains the most cost-effective option.
"A cost of 60,000 euros is the generally accepted amount of money we as a society are willing to pay for one QALY gained," Smits said.
If the sensitivity of selective strategies falls to less than 91%, which is quite feasible given that more than 90% of MHI patient CT scans are "normal" (i.e., show no signs of traumatic abnormality), routine CT scanning becomes the clear dominant strategy, she said.
The results from the study are timely, as the use of selective strategies in mild head injury patients for CT scanning are presently under consideration by several health systems, including Dutch and British authorities.
The U.K.'s National Institute for Health and Clinical Excellence (NICE) has proposed selective scanning based on the CCHR method, while current guidelines in the Netherlands may be revised to allow selective scanning based on NOC. Smits' findings will be taken into account in the Netherlands.
By Rob Skelding
AuntMinnie.com contributing writer
March 7, 2008
Related Reading
Emergency care can equal 1,000 x-rays: study, March 5, 2008
Increased use of CT scans raises risk of higher radiation exposures, November 29, 2007
256-slice CT brings new possibilities in head imaging, May 28, 2007
MRI, CT remain front and center in head trauma imaging, April 18, 2007
Copyright © 2008 AuntMinnie.com

















