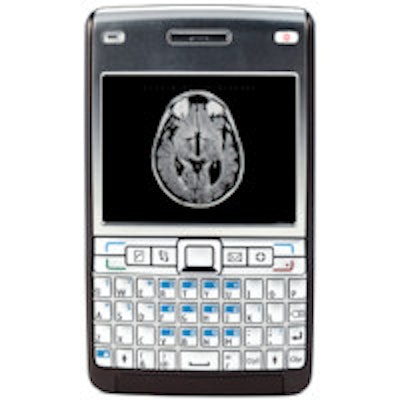
The number of medical imaging-related apps in the marketplace has tripled since January, but that doesn't mean all apps are created equal. Researchers from the U.K. have assessed 321 imaging-related apps, finding that while there are some gems, many others may have questionable content.
Smartphone health-related apps are rapidly increasingly in number, with approximately 1,000 new programs released each month and 142 million annual downloads predicted by 2016, according to a study published in Insights into Imaging (4 August 2013). The majority (85%) of medical professionals use smartphones, and 30% to 50% use apps within their clinical practice.
The degree of medical involvement in the development of radiology-related applications is currently unclear, so Dr. Mark Rodrigues, from the department of radiology at the Royal Infirmary of Edinburgh, and colleagues sought to identify contemporary radiology-related smartphone apps, including teaching, reference, and DICOM viewing software, and assess the level of advertised medical involvement in app development.
They searched six major app stores (Apple, Google Play, Blackberry Mobile Market, Nokia Ovi, Samsung, and Microsoft Windows Marketplace) between 18 and 30 June 2012 using the following terms: radiology, radiation, x-ray(s), computed tomography/CT, magnetic resonance imaging/MRI, ultrasound, nuclear medicine, fluoroscopy, and mammography/mammogram. They recorded app ratings, cost, and medical input in development.
The researchers identified 321 apps. Of these, 158 were "teaching" programs and 96 were "reference" apps. Three of the 29 DICOM viewing apps had U.S. Food and Drug Administration (FDA) clearance for primary diagnosis, while 62% stated they should not be used for primary diagnosis.
Developers of more than a third of apps (36%) claimed that medical professionals were involved in the app development; 76 (24%) of these apps had descriptions that stated that a specific doctor, radiographer, medical physicist, or hospital was involved in their development in publicity information. A further 40 (12%) mentioned unnamed medical professional involvement (such as "radiologist" or "emergency physician").
Guidelines or papers were used in the development of 12 apps (4%); another 12 (4%) apps were designed by radiology or medical societies, such as the Royal College of Radiology (RCR) or the American College of Radiology (ACR); and 37 (12%) were developed by imaging companies (such as Siemens Healthcare or GE Healthcare). Developers of two apps reported the involvement of a named person but did not disclose his or her professional background, while six (2%) stated general terms such as "exam experts;" developers of 136 (42%) apps did not disclose authorship.
"Compared with the previous reports in other specialties, a relatively large number of radiology-related applications were identified," Rodrigues and colleagues wrote. "This probably reflects the general relevance of radiology compared with the previously studied medical fields, as well the rapid growth in medical applications."
The increased accessibility of apps has obvious benefits, but there are concerns about the accuracy of content in medical apps, especially considering the low level of medical professional involvement (i.e., less than half). Also, potential app users cannot determine the accuracy of the program's content prior to purchase, the researchers noted.
App stores do provide short descriptions written by the developers, as well as customer ratings and comments, and a selection of screen shots, but most (61%) of the apps in the study didn't have ratings. Also, 69% of those rated were based on fewer than 10 ratings, reducing the reliability of the customer feedback, they added.
Expert medical input in the development of medical apps may improve reliability, and this input should be clearly stated in the advertising material to allow potential users to make an informed assessment of an apps reliability prior to purchase, according to Rodrigues and colleagues.
Another way of helping users gauge an app's reliability would be to develop a quality "kite mark" for the field, the researchers suggested.
"This might be a role for the RCR or other radiology societies who could give their stamp of approval for products judged fit for the purpose," they wrote.
Regulation of applications
The FDA has released guidance on its intention to regulate a subset of medical applications, including those allowing access to DICOM images, but the guidance is only a recommendation, and full regulatory oversight has not commenced.
Three of the image viewing apps in the study had FDA approval for primary diagnostic use; the remaining 26 image viewing apps without FDA approval should not be used for this purpose, but this was only stated in the publicity information of 62% of the apps.
To gain FDA approval, a medical product must have substantial equivalence to another legally marketed device (i.e., any new technological changes are at least as safe and effective as the predicate device).
"Whilst the software of the mobile PACS applications is very similar or identical to existing PACS systems, the relevant hardware is clearly different (smartphones versus reporting workstation), and this potentially affects the safety of the smartphone application," the authors wrote.
The Medical Devices Directive (MDD) ensures safety and performance of medical devices throughout the European Union, with each member state having its own regulatory framework.
"However, there is currently no consensus between member states over the definition of a medical device and which medical applications should be considered medical devices, leading to uncertainty among application developers and healthcare providers," Rodrigues and colleagues wrote.
Every registered medical device in the EU must carry the CE Mark, signaling that the manufacturer is satisfied the product conforms to the relevant requirements in the relevant legislation.
Most apps, including DICOM viewing programs, are within the lowest risk category, but there is currently very limited use of the CE Mark in the application stores.
"The ability to view full-resolution images remotely has implications for timely diagnosis and treatment; however, the limitations of using smartphones for image interpretation must be considered," the authors noted. Namely, the display, data confidentiality, security concerns, and speed of data transfer and download.
Study disclosures
One of the co-authors is owner of ResearchActive.com, a company that develops medical applications and provides mHealth solutions.