The lack of high-quality annotated datasets required for training, the difficulty of proving technical validation, and the absence of standards for data sharing between digital systems are the three major issues preventing the introduction of artificial intelligence (AI) in daily clinical workflow, two leading European informatics experts have warned.
"Practically, it is very difficult for radiology departments to negotiate contracts for a variety of AI systems and to integrate them all into their IT environment," noted Prof. Elmar Kotter, from the Department of Radiology, University of Freiburg Medical Center, Germany, and Dr. Erik Ranschaert, PhD, a radiologist at Elisabeth-Tweesteden Hospital (ETZ), Tilburg, the Netherlands, in an editorial posted on 14 August by European Radiology.
"It becomes even more difficult when hospitals want to use their own algorithms and integrate them seamlessly into their diagnostic workflow. In this way, the situation is reminiscent of the early nineties, when PACS implementations were hampered by the lack of communication standards and information sharing frameworks such as DICOM and [Integrating the Healthcare Enterprise (IHE)]," they added
Hype over AI?
The number of AI-related abstract submissions to radiology journals and conferences is skyrocketing, reaching 25% of submissions for Radiology in 2019, and AI in radiology is particularly hyped, explained Kotter and Ranschaert, who are respectively vice-president and president of the European Society of Medical Imaging Informatics (EuSoMII).
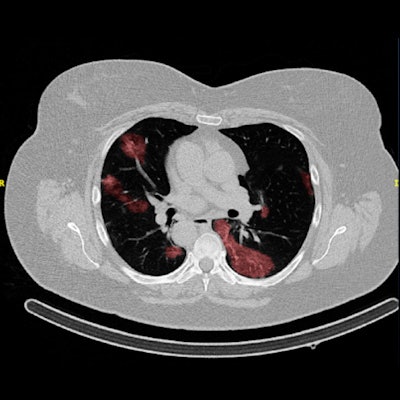
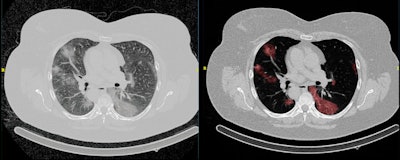 Example of an automated segmentation tool that shows the original image (left) and the predicted segmentation (right). The tool is being used in the Imaging Covid-19 AI research project to develop a deep learning-based model for the automated detection of COVID-19 infection on chest CT and for quantifying lung involvement. The algorithm was trained on a first run of around 1,000 CT scans. Figure courtesy of Quibim.
Example of an automated segmentation tool that shows the original image (left) and the predicted segmentation (right). The tool is being used in the Imaging Covid-19 AI research project to develop a deep learning-based model for the automated detection of COVID-19 infection on chest CT and for quantifying lung involvement. The algorithm was trained on a first run of around 1,000 CT scans. Figure courtesy of Quibim.Many recent publications have shown that AI tools, and especially deep learning, can recognize patterns in medical image data with excellent accuracy.
"We are currently in the transition phase from a mainly morphological to a functional, quantitative, and holistic analysis of image data, supported by rapidly evolving advanced technologies," they wrote. "Within a few decades, systems will become available that think at a human level or higher, allowing us to observe new, as yet unknown phenomena. The radiologist's tasks will be more focused on personalized treatment, including highly specialized and more targeted image-guided tumor biopsies and treatments, and more accurate prediction and evaluation of treatments supported by AI-based analysis of a full spectrum of patient data."
Most radiologists would welcome the support of AI algorithms for many applications, such as the detection and follow-up of lung nodules in CT exams of the chest or the analysis of total body CT scans for the detection and comparison of osteolytic lesions of 5 mm or larger in patients with multiple myeloma. These are repetitive, time-consuming tasks without much satisfaction for the radiologist.
"It is important for the radiological community to focus on defining appropriate use cases, based upon existing needs, thus allowing the developers to train algorithms with a clearly clinical purpose," Kotter and Ranschaert continued. "AI will augment radiologists in this role, and therefore the abbreviation could also be interpreted as 'Augmented Intelligence.' "
Need for active engagement
Radiologists must be actively engaged in the development of ethical and regulatory guidelines for the use and approval of AI tools, and attention must be paid to the possible built-in bias of algorithms, as it may cause unforeseen harm to patients, they noted. To detect significant system errors, the overall integration of AI systems in radiology will need standardized and regulated monitoring of outcomes.
"The time has now come to adopt a proactive attitude and to reevaluate our position as radiologists on the long term," the authors wrote. "The new generation of radiologists should not necessarily become computer experts, but they should have a basic knowledge of the underlying technique so that they can work in partnership with engineers and clinical physicists to train and improve algorithms, preferably with their own data."
AI will not weaken radiologists but rather help them strengthen their function and give them an indispensable role in personalized medical care. Radiologists must acquire sufficient understanding of AI to be able to steer its development and its impact on their profession, and they must therefore become actively involved in this ongoing transformation, in all areas, Kotter and Ranschaert concluded.



















