Supine breast MRI with a lightweight, wearable radiofrequency coil vest (called BraCoil) can offer a significant advantage over prone MRI by providing more accurate lesion positioning relative to ultrasound, a new Austrian study has found.
The approach could improve lesion localization in radiotherapy planning, surgery, targeted ultrasound, and ultrasound-guided biopsy, potentially reducing the need for MR-guided biopsies, first author Lena Nohava, PhD, a postdoctoral researcher at the High Field MR Center and Christian Doppler Laboratory for Patient-Centered Breast Imaging, Medical University of Vienna (MedUni Wien), and colleagues noted in an article posted on 1 February in the European Journal of Radiology (EJR).
"The BraCoil is currently being used in two ongoing clinical studies in Vienna and Nancy, France," corresponding author Elmar Laistler, PhD, head of the Radio Frequency Lab at MedUni Wien, told AuntMinnieEurope.com on 4 February. "It is not yet commercially available, but the second generation coil design intended for commercialization is currently being developed."
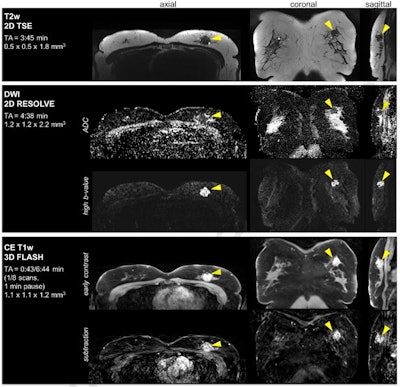 Figure 1. Clinical breast cancer patient data set acquired with the BraCoil in the supine position. MRI shows a 22 mm mass lesion diagnosed as invasive ductal carcinoma. Coronal slice acquisition (i.e., highest in-plane resolution) was used in T2-weighted and diffusion-weighted imaging; axial slice acquisition in dynamic contrast-enhanced T1-weighed imaging. In this patient, the full protocol duration (including localizer scan) was 15 minutes 20 seconds, and seven postcontrast scans were enabled by high parallel imaging acceleration (R = 3 x 3). All figures courtesy of Lena Nohava, PhD, Elmar Laistler, PhD, et al, and EJR.
Figure 1. Clinical breast cancer patient data set acquired with the BraCoil in the supine position. MRI shows a 22 mm mass lesion diagnosed as invasive ductal carcinoma. Coronal slice acquisition (i.e., highest in-plane resolution) was used in T2-weighted and diffusion-weighted imaging; axial slice acquisition in dynamic contrast-enhanced T1-weighed imaging. In this patient, the full protocol duration (including localizer scan) was 15 minutes 20 seconds, and seven postcontrast scans were enabled by high parallel imaging acceleration (R = 3 x 3). All figures courtesy of Lena Nohava, PhD, Elmar Laistler, PhD, et al, and EJR.
The group's main aim was to evaluate the BraCoil for supine breast MRI, comparing lesion displacement and size with standard prone MRI and supine ultrasound, and assess its potential impact on clinical workflows for targeted ultrasound and ultrasound-guided biopsy.
"The custom-built BraCoil has 28 flexible receive channels and is currently being used as a research device in clinical studies at two sites in Europe," explained the researchers, adding that it is compatible with 3-tesla scanners from Siemens Healthineers.
Benchmark tests of the device against a standard breast MR coil in 12 healthy female volunteers with small to large breast volumes showed up to threefold SNR improvement, enabling high-resolution imaging and reliable detection of small lesions. Parallel imaging acceleration with the BraCoil is enabled by its high channel count (both in left-right and head-foot direction). Its design also enhances patient comfort and potentially improves correlation between supine MRI and ultrasound, aiding in targeted ultrasound, biopsy, surgery, or radiotherapy planning.
MRI and ultrasound data were collected from 11 female patients with 18 breast lesions. Patients underwent two MRI exams: standard prone MRI using a commercial coil and supine MRI using the BraCoil. Lesion positions were compared between prone MRI, supine MRI, and supine ultrasound using anatomical landmarks (skin, pectoral muscle, nipple). Statistical analysis was performed on the mean absolute differences in lesion positions.
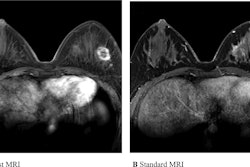
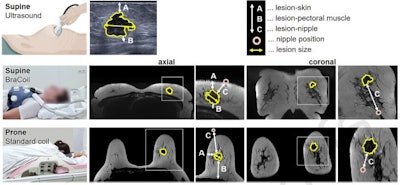 Figure 2. Breast ultrasound and MRI setups and measured distances for lesion description. Lesion skin, lesion-pectoral muscle, lesion-nipple distances (A, B, and C), and lesion size were measured in axial. Lesion-nipple distance was additionally measured in coronal orientation. All distances were taken from the border of the lesion. They represent the shortest distance between the two points in axial and coronal, respectively. In coronal, the lesion-nipple distance is the projected distance also indicating the quadrant. The patient case is identical to the one shown in Figure 1.
Figure 2. Breast ultrasound and MRI setups and measured distances for lesion description. Lesion skin, lesion-pectoral muscle, lesion-nipple distances (A, B, and C), and lesion size were measured in axial. Lesion-nipple distance was additionally measured in coronal orientation. All distances were taken from the border of the lesion. They represent the shortest distance between the two points in axial and coronal, respectively. In coronal, the lesion-nipple distance is the projected distance also indicating the quadrant. The patient case is identical to the one shown in Figure 1.
With ultrasound lesion positions as a reference, supine MRI acquired with the BraCoil showed significantly less lesion displacement compared to prone MRI, with on average 7.3 mm less lesion-skin and 26.7 mm less lesion-pectoral muscle displacement. Lesion-nipple distances in supine MRI showed strong deviations compared to prone MRI. Lesion size in supine MRI was more comparable to ultrasound than prone MRI, but it changed insignificantly across modalities. In total, four out of 18 lesions were only detectable in targeted ultrasound after supine BraCoil MRI.
The authors emphasized that the results presented in this study are preliminary, but they indicate a clear potential to create impact on a larger scale, especially in streamlining the clinical communication of lesion positions between radiologists concerned with different imaging modalities, and surgeons or radio oncologists planning interventions in breast cancer patients.
"For patients, replacing standard prone with supine breast MRI considerably improves comfort and, even more importantly, extends the MR inclusion criteria to immobile, obese or pregnant patients who cannot undergo the prone exam," they stated. "Additionally, the change in positioning avoids the discomfort of having to expose both breasts using the standard rigid coil and can reduce pain in patients with large hematoma post-biopsy or fragile bones post-radiotherapy."
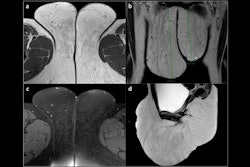
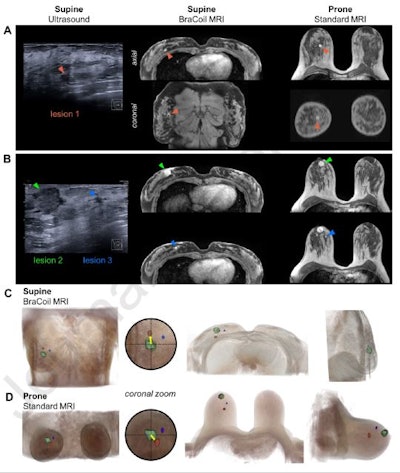 Figure 3. Ultrasound and early contrast-enhanced T1-weighted MRI of a 43-year-old patient (European bra size 85C, U.S. bra size 38 C) diagnosed with multicentric invasive ductal carcinomas -- (A) lesion 1: 6 mm, (B) lesion 2: 20 mm, lesion 3: 4 mm. Arrows mark the lesion positions. 3D renderings of supine BraCoil (C) and prone standard coil MRI at 1.5 T (D) data illustrate the absolute and relative change in lesion positions. The case shows deviating lesion positions between prone and supine MRI due to breast tissue deformation which occurs especially in larger breasts. Here, the change in distance of the lesion to the nipple or pectoral muscle comparing prone and supine MRI and supine ultrasound is clearly noticeable. The 3D renderings depicted in C and D demonstrate that, e.g., in axial, with the lesion marked in green or the nipple as a reference point, the red lesion appears laterally in supine MRI but medially in prone MRI. The coronal view further reveals that relative to the green lesion, in supine MRI the red lesion is located cranially while in prone MRI it appears caudally.
Figure 3. Ultrasound and early contrast-enhanced T1-weighted MRI of a 43-year-old patient (European bra size 85C, U.S. bra size 38 C) diagnosed with multicentric invasive ductal carcinomas -- (A) lesion 1: 6 mm, (B) lesion 2: 20 mm, lesion 3: 4 mm. Arrows mark the lesion positions. 3D renderings of supine BraCoil (C) and prone standard coil MRI at 1.5 T (D) data illustrate the absolute and relative change in lesion positions. The case shows deviating lesion positions between prone and supine MRI due to breast tissue deformation which occurs especially in larger breasts. Here, the change in distance of the lesion to the nipple or pectoral muscle comparing prone and supine MRI and supine ultrasound is clearly noticeable. The 3D renderings depicted in C and D demonstrate that, e.g., in axial, with the lesion marked in green or the nipple as a reference point, the red lesion appears laterally in supine MRI but medially in prone MRI. The coronal view further reveals that relative to the green lesion, in supine MRI the red lesion is located cranially while in prone MRI it appears caudally.
The researchers' aim is for future studies to verify inter-reader agreement of lesion position descriptions, improve coil hardware design and usability, and optimize supine MRI protocols, such as for reliable fat suppression. The visualization of the supine BraCoil data in a panoramic view may further accelerate image reading. Also, the co-registration of the supine BraCoil MRI and ultrasound data may be a helpful add-on to perform ultrasound-guided needle biopsy in cases where MRI-detected breast lesions are still undetectable in targeted ultrasound.
You can read the full EJR article here. The co-authors were Dr. Paola Clauser, PhD, Raphaela Czerny, PhD, Dr. Pascal Baltzer, PhD, and Elmar Laistler, PhD.