Digital breast tomosynthesis (DBT) increased breast cancer detection rates over a 10-year time period, researchers reported in a study published on 17 September in Radiology.
A group led by Dr. Liane Philpotts, from Yale University in New Haven, Connecticut, U.S., also found that DBT identifies invasive cancers with a lower rate of advanced cancers compared with digital mammography. The team added that this further improved on incident rounds of breast cancer screening.
"The improved cancer detection is something for women to think about," Philpotts told AuntMinnieEurope.com. "If they choose to be screened, requesting to go to a site that offers DBT would be in their best interest."
Previous studies have highlighted DBT's performance in increasing breast cancer detection compared to conventional mammography. However, the researchers noted that it's unknown whether this added tumor detection will improve patient outcomes or lead to overdiagnosis.
The Yale team compared cancer types and stages with 10 years of DBT screening and over three years of digital mammography screening. It included data collected between 2008 and 2021 from 1,407 breast cancers. Of these, 1,265 were analyzed via DBT and 142 via mammography.
DBT led to a higher rate of cancer depiction than mammography (5.3 versus four cancers per 1,000; p = 0.001). The researchers added that DBT achieved a similar ratio of invasive cancers to ductal carcinomas in situ (DCIS) compared to mammography, at 76.5% versus 71.1%, respectively.
Among other findings, the modalities did not significantly differ in average invasive cancer size; both had similar rates of invasive cancer subtypes, and DBT had a lower proportion of advanced cancers.
| Comparison between DBT, mammography in 10-year study | |||
|---|---|---|---|
| Measure | Mammography | DBT | p-value |
| Average invasive cancer size | 1.44 cm | 1.36 cm | 0.49 |
| Rates of low-grade cancers | 29% | 26.5% | * |
| Rates of moderate-grade cancers | 51% | 57.2% | * |
| Rates of high-grade cancers | 20% | 16.1% | * |
| Proportion of advanced cancers | 43.6% | 32.6% | 0.04 |
| *The p-value of the rates of invasive cancer subtypes (low, moderate, high grade) between mammography and DBT was 0.65, not achieving statistical significance. | |||
Also, prevalent screening with DBT had a higher proportion of advanced cancers compared to DBT incident screening (39.1% versus 29.1%; p = 0.003). Incident DBT cases were also significantly smaller than prevalent cases (1.2 cm versus 1.6 cm; p < 0.001).
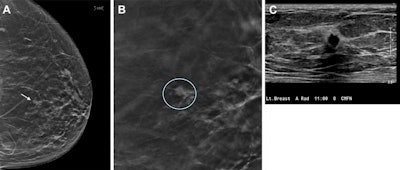 Images depict a 67-year-old woman who was recalled from screening for a small focal asymmetry in the left breast. (A) 2D mammographic image shows the lesion (arrow), which is difficult to see. (B) The digital breast tomosynthesis section image shows spiculated margins (circle). (C) The ultrasound image shows a corresponding irregular hypoechoic mass with angular margins. Pathologic evaluation revealed a 0.7-cm triple-negative invasive carcinoma. Image courtesy of RSNA.
Images depict a 67-year-old woman who was recalled from screening for a small focal asymmetry in the left breast. (A) 2D mammographic image shows the lesion (arrow), which is difficult to see. (B) The digital breast tomosynthesis section image shows spiculated margins (circle). (C) The ultrasound image shows a corresponding irregular hypoechoic mass with angular margins. Pathologic evaluation revealed a 0.7-cm triple-negative invasive carcinoma. Image courtesy of RSNA.Finally, the researchers observed no significant difference in interval cancer rates between mammography (0.14 per 1,000) and DBT (0.2 per 1,000; p = 0.42).
Philpotts said the team is going to next assess how these results compare with different screening intervals. She also called for future studies to do more in-depth analysis on how patient factors such as breast density, age, and ethnicity play into cancer trends as found on DBT.
"It's interesting, because in the U.S., women do one- or two-year intervals depending on recommendations," she told AuntMinnie.com. "We want to lower that advanced cancer rate. We want to optimize it [screening] as much as possible."
In an accompanying editorial, Dr. Soo-Yeon Kim, PhD, and Dr. Ok Hee Woo, PhD, from Korea University Guro Hospital in Seoul wrote that these findings "provide indirect evidence suggesting the potential of DBT screening in improving survival outcomes." However, they added that this is pending confirmation from the results of the Tomosynthesis Mammographic Imaging Screening Trial.
Kim and Woo added that the higher proportion of white participants who underwent DBT in the study compared to Black and Hispanic women suggests that DBT may not be as accessible for the latter.
"As radiologists, it is imperative that we take a leading role in enhancing access to and awareness of proven advanced imaging methods for underserved populations," they wrote.
The full study can be found here.