Using AI with supplemental breast MRI is about four times more efficient at detecting breast cancers than traditional breast density measurement methods, a study published on 8 July in Nature Medicine found.
Researchers led by Dr. Fredrik Strand, PhD, from the Karolinska Institute in Solna, Sweden, found in their analysis of the ScreenTrustMRI trial that using an AI-based score to select a small proportion of women for supplemental MRI after negative mammography detected many missed cancers. They added that this makes the cost per cancer detected comparable with cancers found by screening mammography.
"We found that it is possible to make a very precise selection of women for supplemental MRI based on AI analysis of the negative screening mammograms," Strand told AuntMinnieEurope.com.
Supplemental MRI is a go-to imaging method for assessing women with dense breasts, which conventional mammography struggles to analyze. However, breast MRI’s utility is limited, with the researchers pointing out an overall lack of qualified MRI staff and high costs tied to MRI equipment.
The Strand team conducted a randomized clinical trial, ScreenTrustMRI, using its recently developed AI tool to score each mammogram called AISmartDensity. AISmartDensity has a modular structure with three component models assessing underlying risk, potential masking, and suspicious cancer signs. The researchers highlighted that its primary purpose is to triage women for supplemental MRI after negative screening mammography.
For the study, the team offered trial participation to women with a negative screening mammogram and a high AI score (top 6.9%). Of the 1,211 women included, 559 were randomly assigned to and completed receiving supplemental MRI and 652 were not assigned to MRI.
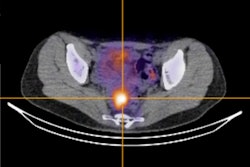
 (A) Case A was a 13-mm large BI-RADS 4 finding on MRI that corresponded to a 13-mm large invasive cancer as diagnosed in the surgical specimen. (B) Case B was a 9-mm large BI-RADS 4 finding on MRI that corresponded to an 8-mm invasive cancer and 14-mm ductal cancer in situ. (C) Case C was three suspicious lesions within a total area of 60 mm, BI-RADS 5 finding on MRI, that corresponded to a 50-mm multifocal invasive lobular cancer. (D) Case D was two suspicious lesions, the largest 13 mm, BI-RADS 3 on MRI, which corresponded to a 10-mm invasive lobular cancer with 85-mm extent including ductal cancer in situ. Images courtesy of Nature Medicine. Licensed under CC BY 4.0.
(A) Case A was a 13-mm large BI-RADS 4 finding on MRI that corresponded to a 13-mm large invasive cancer as diagnosed in the surgical specimen. (B) Case B was a 9-mm large BI-RADS 4 finding on MRI that corresponded to an 8-mm invasive cancer and 14-mm ductal cancer in situ. (C) Case C was three suspicious lesions within a total area of 60 mm, BI-RADS 5 finding on MRI, that corresponded to a 50-mm multifocal invasive lobular cancer. (D) Case D was two suspicious lesions, the largest 13 mm, BI-RADS 3 on MRI, which corresponded to a 10-mm invasive lobular cancer with 85-mm extent including ductal cancer in situ. Images courtesy of Nature Medicine. Licensed under CC BY 4.0.
The study found that 36 of the women had cancerous lesions detected, corresponding to 64.4 cancers found per 1,000 MRI exams. The Dense Tissue and Early Breast Neoplasm Screening (DENSE) trial meanwhile showed a cancer detection rate of 16.5 per 1,000 MRI exams.
Also, the proportion of cancers identified in women recalled after MRI (positive predictive value [PPV1]) was 37.9%. For women assessed as BI-RADS 3, 4, and 5, the PPV1 was 13%, 63%, and 85.7%, respectively. The proportion of cancers among biopsied women meanwhile was 50.7%.
The median size of the only or the largest malignant lesion measured on MRI was 12 mm, with the total extent of malignancy ranging between 7 and 85 mm. On histopathological analysis of surgical specimens, 22 (61%) were a combination of invasive and ductal cancer in situ (DCIS), with five being in situ only.
Finally, the researchers highlighted that using AISmartDensity would make the detection cost per cancer similar to the cost of population-wide screening mammography and contribute to earlier detection of invasive cancer. They cited a cost-effectiveness study that estimated the cost per quality-adjusted life years (QALY) gained for supplemental MRI every three years at €37,181.
"Given the high cancer yield and diverse cancer characteristics in our study we expect that it was valuable to find these cancers now, and not two years later at the next screening or as interval cancers before that," Strand said.
The study authors wrote that an assessment of this approach is planned as a post hoc reader study. They also highlighted that subsequent follow-up research will determine primary outcomes of this AI approach on prognostically important cancer characteristics.
Strand told AuntMinnieEurope.com that the team is setting up a spinoff company to work on obtaining regulatory approval for AISmartDensity.
The study can be found in its entirety here.