Ultrasound elastography shows differences in placental stiffness between pregnant women who recovered from COVID-19 compared with women with no history of COVID, a Turkish study published on 23 August in Placenta found.
A team led by Dr. Bedri Sakcak from Ankara City Hospital calculated point shear-wave velocity from ultrasound elastography scans and found that pregnant women who recovered from COVID-19 have more rigid placentas. What's more, newborns born to these women needed intensive care.
"The use of point shear wave velocity... may provide valuable information in the diagnosis and management of post-COVID-19 patients as a complementary tool to the existing ultrasonography methods," Sakcak et al wrote.
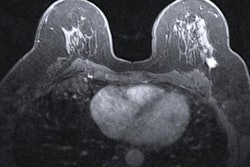
The health of the placenta plays a role in fetal and maternal morbidity and mortality, with tissue elasticity measurements helping with assessment of underlying pathologies. Elastography is used in ultrasound imaging in oncology settings to determine the stiffness of tissues and organs, with diseased tissue typically being stiffer than healthy tissue. Sonoelastography is a noninvasive technique that can be used to analyze the elasticity of parenchymal tissue.
Previous research suggests that the prevalence of obstetric complications such as stillbirth and fetal distress have increased since the beginning of the COVID-19 pandemic. Studies have also suggested that COVID-19 may cause maternal and fetal complications.
The researchers noted a lack of data regarding the elasticity of the fetal placenta, adding that higher shear-wave velocity values in previous studies indicated stiffer tissue.
Sakcak and colleagues wanted to add literature to this area, exploring placental changes in point shear-wave velocity on sonoelastography between pregnant women who recovered from COVID-19 and women without a history of COVID-19. They used a technique called virtual touch tissue quantification, which is based on acoustic radiation force impulse to measure tissue elasticity.
The team used the technique to calculate shear-wave velocity in meters per second (m/s), with higher values indicating that the elastography traveled more quickly through the tissue -- a sign of higher stiffness.
The study authors prospectively looked at data from a total of 80 women. The COVID-19 recovery and control groups were split evenly at 40 women each. The women had an age range between 18 and 44 years.
| Differences in elastography measures between pregnant women who recovered from COVID-19 and women with no history of COVID-19 | ||
| Women with no COVID history | Women in COVID recovery group | |
| Point shear-wave velocity (average) | 1.77 m/s | 1.9 m/s |
| Uterine artery pulsatility index (average) | 0.77 | 0.96 |
| Apgar score (average) | 7.3 | 6.9 |
| Newborn intensive care unit needed | 2 births | 11 births |
The researchers also found that 31 women in the COVID recovery group had placental lacunae, vascular lakes seen within placental parenchyma. Meanwhile, just one woman in the no-history group had a placental lacuna.
The team also found a positive and significant correlation between having a history of COVID-19 and shear-wave velocity (r = 0.28, p = 0.01) and the presence of placental lacunae (r = 0.28, p = 0.01). The group also found negative and significant correlations between body mass index and shear wave velocity (r = -0.22, p = 0.04) and between gestational week and shear wave velocity (r = -0.31, p = 0.004).
No statistically significant differences were found in the placental shear-wave velocity measurements of the post-COVID-19 group according to hospitalization, steroid use, or receiving medical treatment.
The authors wrote that point shear-wave velocity via elastography can contribute "a new diagnostic technique" for pregnant women with a history of COVID-19. They added that it can be potentially used on women with gestational diabetes, preeclampsia, placental invasion anomalies, or other diseases considered to be affected by the placenta due to inflammation or fibrosis during pr