MRI allows precise evaluation of rare vulvar pathologies, differentiating benign from malignant lesions, and is crucial for tailored clinical approaches, researchers have reported.
"A comprehensive understanding of vulvar anatomy in MRI facilitates the correct diagnosis of lesions and improves disease extent detection for surgical planning," noted lead authors Dr. Paola Clauser, from the Department of Biomedical Imaging and Image-guided Therapy, Division of General and Pediatric Radiology, Medical University of Vienna, and Dr. Miriam Dolciami, from the Department of Diagnostic Imaging, Radiation Oncology and Hematology, Fondazione Policlinico Universitario Agostino Gemelli IRCCS, Rome.
 A 37-year-old woman presented with a nodule above the clitoris that was slow-growing for 10 years but which had recently become painful. Axial (a) and coronal (b) T2WI show an oval, well-defined vulvar mass (white arrow) involving the clitoral glans without invasion of adjacent organs with a hyperintense, heterogeneous signal. The lesion presents diffusion restriction on DWI (c) and the corresponding ADC map (d). Axial contrast-enhanced axial fat-saturated T1WI shows heterogeneous enhancement (e). The lesion was removed surgically, and the final diagnosis was schwannoma. All images courtesy of Drs. P. Clauser, M. Dolciami, B. Gui et al and EJR.
A 37-year-old woman presented with a nodule above the clitoris that was slow-growing for 10 years but which had recently become painful. Axial (a) and coronal (b) T2WI show an oval, well-defined vulvar mass (white arrow) involving the clitoral glans without invasion of adjacent organs with a hyperintense, heterogeneous signal. The lesion presents diffusion restriction on DWI (c) and the corresponding ADC map (d). Axial contrast-enhanced axial fat-saturated T1WI shows heterogeneous enhancement (e). The lesion was removed surgically, and the final diagnosis was schwannoma. All images courtesy of Drs. P. Clauser, M. Dolciami, B. Gui et al and EJR.
Pathologies of the vulva are rare, with vulvar malignancy comprising 2%-4% of female tract cancers. Most are squamous cell carcinomas, but benign and malignant lesions of epithelial and mesenchymal origins may also occur, they explained in an article posted on 13 January by the European Journal of Radiology (EJR).
Melanocytic lesions, hematolymphoid proliferations, neuroendocrine tumors, and metastatic lesions may exist. Diagnosis is based on histopathological evaluation, but imaging can play a key role in guiding treatment by allowing a precise staging of malignant pathologies and evaluation of the disease extent and its relationship with the surrounding structures before surgery. Clinical evaluation can be complex due to mass and discomfort, especially when evaluating deep structures, according to the authors.
"It is also interesting to note that vulvar morphology changes throughout a person's lifetime, primarily influenced by hormone levels," they explained, adding that during puberty, there is an accumulation of adipose tissue in the mons pubis and the labia majora, clitoris, and labia minora become more prominent, the vaginal introitus increases in diameter, and the urethral orifice becomes more visible. After menopause, the labia majora loses subcutaneous fat, the clitoris decreases in volume, and both the labia minora and vaginal introitus undergo atrophy.
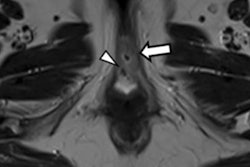
 High-resolution axial T2 images show the clitoris (white arrows) of a 16-year-old post- pubertal woman (a) and a 73-year-old post-menopausal woman (b). In the younger woman, the clitoris is prominent and has a higher signal in T2 weighted images (WI); in the older woman, it is reduced in volume and has a lower signal in T2WI.
High-resolution axial T2 images show the clitoris (white arrows) of a 16-year-old post- pubertal woman (a) and a 73-year-old post-menopausal woman (b). In the younger woman, the clitoris is prominent and has a higher signal in T2 weighted images (WI); in the older woman, it is reduced in volume and has a lower signal in T2WI.
The recommended MRI protocol for local staging of vulvar lesions includes T2WI, diffusion-weighted imaging (DWI), and dynamic contrast-enhanced sequences of the pelvis. For patient preparation, fasting, administration of antispastic agents, and emptying the bladder before the examination are recommended, while vaginal gel opacification is optional. The minimum recommended magnet field strength is 1.5 tesla, and the patient should be examined supine.
In 2021, the European Society of Urogenital Radiology (ESUR) provided the most recent and accepted recommendations for vulvar MRI, focusing on vulvar cancer staging, Clauser and Dolciami pointed out.
 A 48-year-old woman who had already undergone a hysterectomy for multiple leiomyomas, presented with palpable masses at the level of the left labia minora and vagina. MRI shows multiple oval and round, well-defined masses at the level of the vulva, vagina, perianal, and perirectal. These lesions show hypointense signal intensity on sagittal (a) and axial (b) T2WI, with diffusion restriction on high b-value diffusion-weighted imaging (c) and ADC map (d), and homogeneous late enhancement in axial post-contrast fat-saturated T1WI (e). The final histologic diagnosis was extrauterine leiomyomas.
A 48-year-old woman who had already undergone a hysterectomy for multiple leiomyomas, presented with palpable masses at the level of the left labia minora and vagina. MRI shows multiple oval and round, well-defined masses at the level of the vulva, vagina, perianal, and perirectal. These lesions show hypointense signal intensity on sagittal (a) and axial (b) T2WI, with diffusion restriction on high b-value diffusion-weighted imaging (c) and ADC map (d), and homogeneous late enhancement in axial post-contrast fat-saturated T1WI (e). The final histologic diagnosis was extrauterine leiomyomas.
In malignancies, imaging of the upper abdomen using T2 Half Fourier Single-shot Turbo spin-Echo (HASTE) and DWI sequences in the axial plane is also recommended to assess kidney involvement and lymphadenopathy.
"Multiplanar evaluation is essential to evaluate all the vulvar components, including the coronal plane for minor and major labia and the sagittal plane for the urethral meatus," the authors wrote. "The anatomy of the clitoris is better assessed on the axial plane. Artifacts from air presence between vulvar components can affect diffusion sequences and must be considered during image evaluation."
 Childhood asymmetrical labium majus enlargement (CALME). A 30-year-old woman presented with hypertrophy of the external genitalia without skin alterations or symptoms. Axial (a), coronal (b), and sagittal (d) T2WI reveal hypertrophic subcutaneous adipose tissue (both superficial and deep) in the vulvar area, particularly at the level of the mons pubis and the labia majora (right > left). Axial fat-saturated T2WI (c) confirms adipose hypertrophy without signs of heteroplastic tissue or lymphoedema. The final diagnosis was late-onset CALME.
Childhood asymmetrical labium majus enlargement (CALME). A 30-year-old woman presented with hypertrophy of the external genitalia without skin alterations or symptoms. Axial (a), coronal (b), and sagittal (d) T2WI reveal hypertrophic subcutaneous adipose tissue (both superficial and deep) in the vulvar area, particularly at the level of the mons pubis and the labia majora (right > left). Axial fat-saturated T2WI (c) confirms adipose hypertrophy without signs of heteroplastic tissue or lymphoedema. The final diagnosis was late-onset CALME.
Vulvar anatomy and pathologies are still not very well known by radiologists because they are very rare pathologies, corresponding author Dr. Benedetta Gui, a radiologist at Fondazione Policlinico Universitario Agostino Gemelli IRCCS, told AuntMinnieEurope.com.
To ensure widespread distribution of the EJR article, the researchers opted for open access. You can read the full article here.