The European Society of Urogenital Radiology (ESUR) has issued new MRI guidelines in a bid to reduce ambiguity and improve radiology's role in the staging and management of patients with vulvar cancer.
The ESUR's Female Pelvic Imaging Working Group comprising 21 experts from 20 different institutions developed the guidelines after noting a lack of standardized recommendations, even though MRI has emerged as the clear modality of choice for evaluating local growth of vulvar cancer.
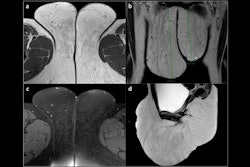
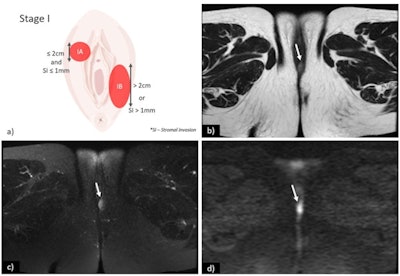 (a) Schematic illustration of International Federation of Gynaecology and Obstetrics (FIGO) stage I. Axial T2-weighted image (b), axial fat saturation T2-weighted image (c) and diffusion-weighted imaging with b-value = 800 s/mm2. (d) shows a vulvar tumor measuring < 2 cm, with pathologic proven stromal invasion of 4 mm, corresponding to FIGO stage IB. All images courtesy of Dr. Olivera Nikolić and Insights into Imaging.
(a) Schematic illustration of International Federation of Gynaecology and Obstetrics (FIGO) stage I. Axial T2-weighted image (b), axial fat saturation T2-weighted image (c) and diffusion-weighted imaging with b-value = 800 s/mm2. (d) shows a vulvar tumor measuring < 2 cm, with pathologic proven stromal invasion of 4 mm, corresponding to FIGO stage IB. All images courtesy of Dr. Olivera Nikolić and Insights into Imaging."In spite of that, MRI staging of vulvar cancer is not used routinely in all cancer centres," the group's chair, Dr. Olivera Nikolić of the University of Novi Sad, Serbia, and colleagues wrote in an article published on 22 September in Insights into Imaging. "Standardising image acquisition techniques and MRI interpretation reduces ambiguity and ultimately improves the contribution of radiology to the staging and management of patients with vulvar cancer."
Diagnosis of vulvar cancer
Vulvar cancer is a rare gynecologic malignancy primarily affecting postmenopausal women, with squamous cell carcinomas (SCC) accounting for approximately 85% of vulvar cancers.
Initial diagnosis of vulvar cancer is made by gynecological examination and biopsy. The final diagnosis is established by histological examination of the primary tumor and lymph node specimens. Given its excellent contrast resolution, MRI is considered the imaging modality of choice for evaluating local growth of vulvar cancer and to exclude invasion of nearby situated organs.
Nikolić and colleagues designed a questionnaire of 54 questions covering indications and technical details, minimal hardware characteristics, patient preparation, and examination protocols and reporting, and sent it out to 21 experts in the field. For some questions, multiple answers were possible.
Responses to the questionnaire with an agreement equal to or more than 80% were considered. Additionally, the authors conducted a literature review to complement and further support their conclusions.
In most cases of vulvar cancer, patients present at an early stage with vulvar tumefaction or ulcer that may be associated with pain, pruritus, bleeding, or discharge. Metastatic involvement of the inguinofemoral lymph nodes is the most important prognostic factor and influences the surgical approach and the need for chemoradiation therapy, the team noted.
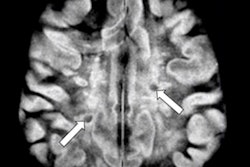
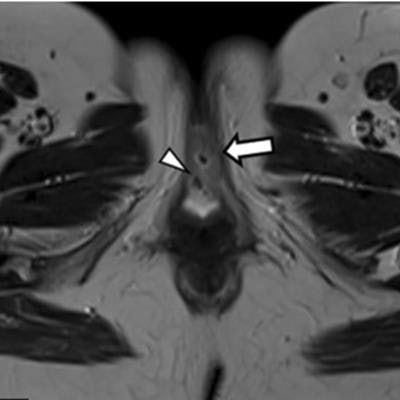
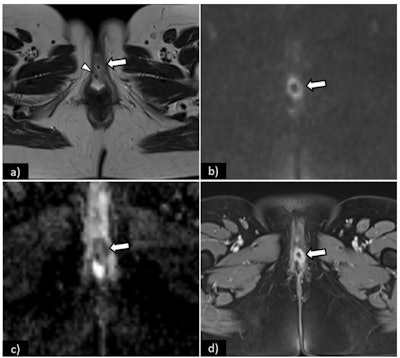 Axial T2-weighted image (a) shows an intermediate signal intensity tumor (arrow), measuring 3 cm, with central necrosis and invasion of the external urethral meatus (arrowhead) -- FIGO II. On diffusion-weighted imaging, the tumor is depicted by a high signal intensity lesion (b-value = 1000 s/mm2) (arrow), and low signal intensity on the corresponding ADC map (arrow). On T1WI fat saturation contrast-enhanced sequence (D), the tumor shows early arterial enhancement of its solid component (arrow), with no enhancement of the central necrotic portion. Note the increased conspicuity of the lesion in diffusion-weighted MRI (b) and (c) and in DCE-MRI (d).
Axial T2-weighted image (a) shows an intermediate signal intensity tumor (arrow), measuring 3 cm, with central necrosis and invasion of the external urethral meatus (arrowhead) -- FIGO II. On diffusion-weighted imaging, the tumor is depicted by a high signal intensity lesion (b-value = 1000 s/mm2) (arrow), and low signal intensity on the corresponding ADC map (arrow). On T1WI fat saturation contrast-enhanced sequence (D), the tumor shows early arterial enhancement of its solid component (arrow), with no enhancement of the central necrotic portion. Note the increased conspicuity of the lesion in diffusion-weighted MRI (b) and (c) and in DCE-MRI (d).The new guidelines apply to adults over 18 who have SCC of the vulva and do not address patients with other vulvar cancer histologies.
The group's key findings include the following:
- MRI is the modality of choice for local staging of vulvar cancer.
- T2-weighted imaging, diffusion-weighted MRI, and dynamic contrast-enhanced MRI are recommended.
- The most widely accepted criterion for inguinofemoral lymphadenopathy is short axis > 1 cm.
- The most specific criterion for inguinofemoral lymphadenopathy is the presence of necrosis.
In addition, the working group reached a unanimous agreement on the need for a structured MRI report in order to improve report quality and to assist with the communication of clinically relevant information to referring physicians.
The team said that MRI reports in vulvar cancer staging should address the following points:
- Tumor size (greatest dimension)
- Tumor location (lateral, midline, multifocal)
- Clitoris involvement when present
- Relationship with adjacent perineal structures: urethra and vagina (lower third or upper part) and anus
- Bladder/rectal invasion
- Inguinofemoral lymph nodes status
- Pelvic lymph nodes status
- Other genital organs (uterus, cervix, vagina, and ovaries)
The most widely used staging system for vulvar cancer was developed by the International Federation of Gynaecology and Obstetrics (FIGO) and revised last in 2009 in close collaboration with the American Joint Commission on Cancer and the Union of International Cancer Control.
"The authors' recommendations on the initial staging of vulvar cancer are in accordance with the latest revision of the FIGO classification," the team concluded.