Structural features tracked on brain MR imaging after patients undergo stereotactic radiotherapy (SRT) for metastatic cancer can help clinicians predict whether tumors will recur, according to a study published on 20 August in Cancer Imaging.
The findings could improve the management of patients with brain metastases, wrote a team led by Beatriz Ocaña-Tienda, PhD, of University of Castilla-La Mancha in Ciudad Real, Spain.
"The development of noninvasive imaging biomarkers might improve patient selection and help in identifying potential nonresponders, as patients may need early treatment adjustments or salvage treatments if they are found to be at a high risk of failure," the group explained.
Brain metastases are the most common type in adults, and their incidence is increasing -- due in part to better detection of small lesions, Ocaña-Tienda and colleagues noted. SRT is the treatment of choice for managing these tumors, but some lesions recur after the radiotherapy course. And at the treatment planning stage, which metastases will recur is unclear, they explained. To address the knowledge gap, the team conducted a study to identify any MR imaging biomarkers that could predict which patients are at a higher risk of recurrence and thus help develop effective treatment protocols.
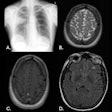
The group analyzed a set of structural brain features found on contrast-enhanced (CE) T1-weighted MR images in 128 patients who were treated with SRT for metastatic brain tumors (57% underwent a single fraction protocol, while 43% underwent fractionated radiotherapy). Of the 183 lesions identified in the study cohort, the majority (58.6%) originated from non-small cell lung cancer (NSCLC) and breast cancer (20.3%), and most patients (49.2%) had only one metastasis. Ocaña-Tienda and colleagues tracked metastatic tumor features such as surface regularity, total volume, presence or absence of necrotic tissue and its volume, and the width of the contrast-enhanced rim.
Overall, the investigators found that total and necrotic tumor volumes and the CE rim width measured at the first follow-up (3 months after treatment) showed statistical significance as imaging biomarkers to predict tumor recurrence.
| Statistically significant MRI-identified imaging biomarkers associated with predicting metastatic brain tumor recurrence at 3 months follow-up | ||
|---|---|---|
| Marker | p-value | Hazard ratio (with 1 as reference) |
| Total volume (cm3) | < 0.001 | 3.5 |
| Necrotic volume (cm3) | 0.004 | 3 |
| CE rim width (cm) | < 0.001 | 2.6 |
The results could translate to better patient care, according to the authors.
"This study illustrated that geometric features derived from [contrast enhanced]-T1w MR images at the first follow-up, approximately three months post-treatment, can serve as predictive indicators for recurrence in BMs following SRT," they concluded.
The complete study can be found here.