Combining theranostics and radiomics – a new concept termed “theragnomics” – could be the key to realizing the full potential of molecular imaging of cancer patients, according to a presentation delivered on 28 February at ECR 2024.
Dr. Desiree Deandreis of Gustave Roussy Cancer Treatment Center in Villejuif, France, described the concept and noted that its goal is to harness imaging power to improve patient selection for treatment, identify how patients respond to therapy, integrate new prognostic biomarkers, and ultimately improve the efficacy of new treatments.
“My question is all the ways we can shift from a simple theranostic model to a complex model,” she told session attendees.
Theranostics is itself a portmanteau of "therapy" and diagnostics" and refers to the dual approach of using the same molecular ligands to both image and treat cancer. It is a relatively simple concept that can be summed up by the expression “see what you treat and treat what you see,” Deandreis explained.
Promising examples of the approach include the use of prostate-specific membrane antigen (PSMA) PET imaging and drugs such as Pluvicto (lutetium-177 [Lu-177] prostate-specific membrane antigen [PSMA]-617), a radioligand therapy approved in the U.S. in 2022.
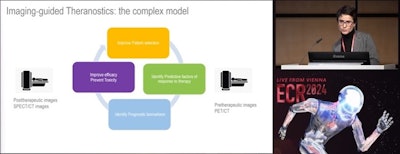 Desiree Deandreis, MD, discussed the development of a more complex theranostics model that integrates radiomics at ECR 20204 in Vienna.
Desiree Deandreis, MD, discussed the development of a more complex theranostics model that integrates radiomics at ECR 20204 in Vienna.
Combining this approach with radiomics – the extraction of data from medical imaging beyond what doctors can visualize with the naked eye – can take theranostics to a new level, according to Deandreis. These radiomics features, such as metabolic tumor volume (MTV) based on PSMA radiotracer uptake by tumors, have been shown to change between patients responding to treatment and those who do not.
New tools will have to be developed to integrate all of the data, and for that researchers are looking to AI, she added.
“The following step is to integrate all these biomarkers that we can extrapolate by images in prognostic and predictive models using, for example, machine learning or deep learning AI,” she said.
Advances in technology will lend themselves to these efforts, such as new techniques in multiparametric PET/CT imaging and the development of new SPECT cameras that offer 3D whole-body views of patients. These advances may allow clinicians to follow the kinetics of radiotracers from the initial injection to their final distribution throughout a patient’s body.
“There is a lot of attention and interest about the total-body PET/CT that is a completely different machine compared to standard PET,” Deandreis said.
AI could play a key role in these technological developments by helping doctors obtain rapid image acquisitions and more efficient calculations when analyzing the results, Deandreis noted. Ultimately, the outcome of these efforts could be the development of “molecular signatures” that may be specific to individual patients and serve as valuable tools for clinicians.
Still, these efforts are in the early stages, and much more work lies ahead, according to Deandreis.
“Now we have to wait for validation of course and standardization then in clinical practice,” she concluded.