A group of orthopedic surgeons in the Netherlands are convinced that medical staff with access to PET/MRI should consider the hybrid modality over other imaging techniques for diagnosing patients with suspected chronic osteomyelitis.
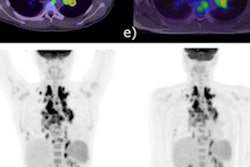
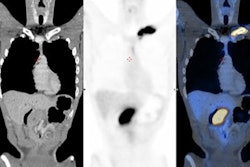
Physicians at Maastricht University Medical Centre have routinely been using PET/MRI scans to plan surgery for patients with chronic osteomyelitis since they published a case series comparing its accuracy to that of PET/CT in 2019. In a recent follow-up study in 36 patients, they suggest evidence that backs up that decision.
"F-18 FDG PET/MRI has the advantages of reduced radiation dose, more soft tissue information, and is deemed more valuable for surgical planning compared to F-18 FDG PET/CT," wrote corresponding author Dennis Hulsen, a medical physicist and orthopedic surgery researcher, and colleagues. The research was published on 1 August in the European Journal of Hybrid Imaging.
Chronic osteomyelitis is a severe and sometimes incapacitating infection of bone and bone marrow that can last for years and that often requires surgical debridement to prevent bone deterioration. Clinical diagnosis is challenging, and imaging plays a key role in identifying the infected areas.
Since they were introduced about 12 years ago, hybrid PET/MRI scanners have proven superior to other imaging techniques for diagnosing orthopedic infections, given their unique combination of metabolic imaging from PET with high-resolution soft-tissue imaging from MRI. To date, approximately 115 of these scanners are available worldwide.
In the current study, the researchers aimed to further explore the use of the technology by evaluating the accuracy of F-18 FDG PET/MRI imaging for diagnosing suspected chronic osteomyelitis in a group of patients.
A nuclear medicine physician and a radiologist, both trained for musculoskeletal imaging, studied images from 36 patients referred for PET/MRI for suspected chronic osteomyelitis between 2015 and 2020 at the Maastricht University Medical Centre. Osteomyelitis was confirmed in all cases based on subsequent positive intraoperative bone microbiology or radiological follow-up of at least one year.
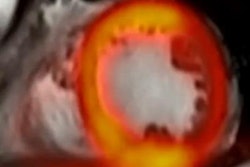
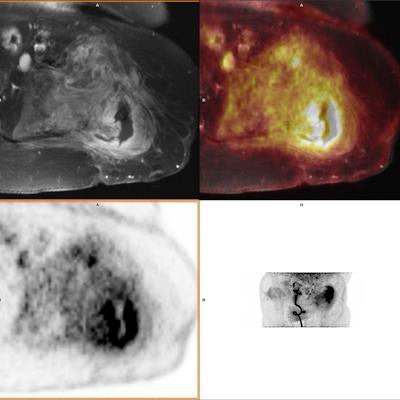
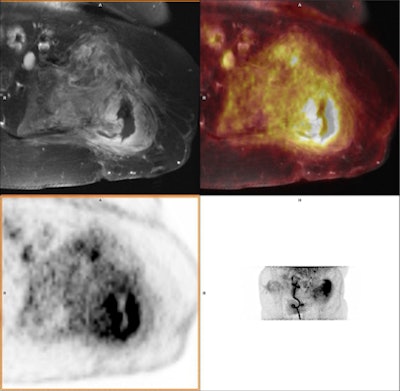 A 43-year-old male with a 20-year-old complex bone injury. The proximal femur was destructed and soft tissue around the bone showed high FDG uptake. PET and MRI conclusions were consistently positive for osteomyelitis. In this case, the extent of the infection based on PET/MRI guided the clinician planning surgery. The presence of osteomyelitis was confirmed by both intraoperative cultures and follow-up. Image courtesy of the European Journal of Hybrid Imaging.
A 43-year-old male with a 20-year-old complex bone injury. The proximal femur was destructed and soft tissue around the bone showed high FDG uptake. PET and MRI conclusions were consistently positive for osteomyelitis. In this case, the extent of the infection based on PET/MRI guided the clinician planning surgery. The presence of osteomyelitis was confirmed by both intraoperative cultures and follow-up. Image courtesy of the European Journal of Hybrid Imaging.Based on the interpretations of the two readers, F-18 FDG PET/MRI yielded 13 true-negative (TN), 18 true-positive (TP), five false-negative (FN), and zero false-positive (FP) cases. Subsequent statistical analysis revealed a sensitivity of 78%, a specificity of 100%, and an accuracy of 86%, according to the results.
"The results are in the same range and not statistically different compared to the diagnostic value for F-18 FDG PET/CT imaging of osteomyelitis in the literature," the authors wrote.
However, in addition, the researchers measured standardized uptake values (SUV) by means of receiver operating characteristics (ROC), which revealed an area under the ROC curve of 0.736 for SUVmax -- a higher AUC for SUVmax than reported in literature for F-18 FDG PET/CT, they noted.
Given this, as well as the integral advantages of PET/MRI over PET/CT of reduced radiation dose and additional soft-tissue information for surgical treatment planning, the researchers suggest PET/MRI has an edge.
"The authors therefore advise physicians with a PET/MRI scanner available to consider it as an alternative for F-18 FDG PET/CT in osteomyelitis diagnosis, while continuously evaluating its value," Hulsen and colleagues concluded.