LONDON - What do circus tricks and a top British boy band have in common? Both had a major impact on the development of imaging during the second half of the 20th century, Dr. Stavros Stivaros, PhD, told the audience at last week's U.K. Royal College of Radiologists (RCR) annual public lecture.
"To start with, x-ray imaging was a parlor or circus trick -- people went to see this as a new invention," said Stivaros, adding that when he was growing up in Lancashire during the 1970s, a Blackburn shoe shop had an x-ray machine for children's feet. "How things have changed!" he declared.
 Times have changed since Dr. Stavros Staviros grew up and shoe shops had x-ray machines.
Times have changed since Dr. Stavros Staviros grew up and shoe shops had x-ray machines.Taking the attendees on an enthralling journey through radiology history up to some of the most recent advances in physiological imaging, Stivaros, National Institute for Health Research (NIHR) clinician-scientist, and senior lecturer at the University of Manchester, had a fun title for his lecture: "From circus trick to space flight: How a British boy band changed neuroimaging forever."
He set the scene by relating the weird and wonderful discoveries that have brought radiology to where it is today. In the very early days, a patient's abnormality was simply photographed, he explained to a packed audience composed of the general public, radiology students, and leading specialists. But in 1895, the field surged ahead when the German physicist, Wilhelm Roentgen, found that when an electron beam was fired at a tungsten atom, x-rays were generated.
In 1917, a woman who had had an operation on her eye later complained that her head felt "sloshy," Stivaros explained. An x-ray determined the presence of air in the cranial vault and this was found to provide contrast, so the brain was visible, outlined by the air. The U.S. neurosurgeon William Dandy further developed this by injecting air into the ventricles, enabling imaging of the brain via an air encephalogram.
Ultrasound was the first modality developed that is still widely used in today's practice. Its origins lie in 1950s Glasgow in Scotland, when an engineer called Tom Brown, who used ultrasound for ship-building, started working with an obstetrician, Ian Donald, and applied it to pregnant women. This was the first time cross-sectional imaging was used, according to Stivaros.
The boy-band connection
Stivaros then explained the boy band connection, and how the music producer, EMI, used earnings from the Beatles' worldwide hits to fund Godfrey Hounsfield, who consequently developed the CT scanner. "This was the start of proper cross-sectional imaging," he said.
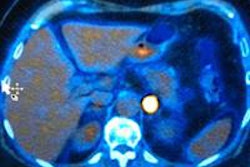
Back then, however, if you wanted to take a serious image of a child with a brain abnormality, the options were limited, mainly due to the lack of contrast between the components of the cranial vault. "It is full of cerebrospinal fluid (CSF), blood, and brain, which all have a similar attenuation to water, so no contrast was visible at this time," elaborated Stivaros, who is also an honorary pediatric neuroradiologist at the Royal Manchester Children's Hospital.
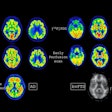
With the arrival of the MRI scanner in the 1980s, courtesy of Paul Lauterbur from the State University of New York at Stony Brook, U.S., and Peter Mansfield from Nottingham University, U.K., the audience was brought up to date with the most significant technologicaladvances in the field. Until relatively recently, most imaging advances have been related to an increase in resolution, but radiology is now entering an exciting era of physiological imaging, Stivaros remarked.
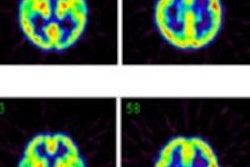
"Using techniques such as diffusion and arterial spin labeling, we can assess cellular packing and brain blood perfusion. Phase contrast MRI allows us to image arterial blood entering the head, venous exiting blood, and CSF flow all noninvasively with no contrast injection," he said.
Pediatric gains
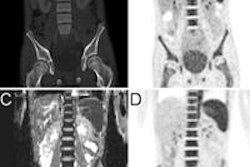
Specifically highlighting advances in pediatric neuroimaging, Stivaros discussed hydrocephalus as a case in point. Affecting 0.82 people per 1,000, it is not insignificant, and has long been considered simply either as an "obstructive outflow problem or communicating and resultant from poor absorption, but we could never assess this in any shape or form." Now, his research group funded by the NIHR is developing quantitative techniques using phase-contrast MRI in children including a noninvasive method of measuring intracranial pressure.
"Using phase-contrast MRI, blood flow into the brain can be measured," he explained. "And because space is occupied by inflowing blood, then CSF and venous blood exits. The time delay on this allows for the calculation of intracranial pressure."
It is hoped this noninvasive technique could aid the follow-up of patients who have had ventriculostomy or shunts for hydrocephalus and experience continued problems. A combination of phase-contrast MRI and arterial spin labeling can determine whether any remaining or new issues such as headaches are related to changes in intracranial pressure, according to Stivaros.
Looking ahead, he added that if the method was approved and entered wide-scale use, then children would be able to avoid lengthy monitoring involving five-day stays in hospital and invasive brain pressure monitoring. It's less invasive, less costly, and can be done on any modern National Health Service (NHS) MRI machine, he said.
Results from the trial are due to be presented at the upcoming RSNA 2014 meeting in Chicago. Until now, most clinicians and researchers have believed that to do this quantitatively, it is necessary to have ECG electrodes on the body, but now this can be done with a finger probe only. This is a huge benefit for a child and a practical step forward for clinicians and staff caring for young patients, Stivaros pointed out.
Coping with practical difficulties
A large part of the challenge with children relates to the practical issues of conducting an MRI exam of a child; their disease processes are entirely different, and scanning them is different too, he explained. "If you've gone to the effort of getting the child onto the scanner then you tend to do lots of imaging. We have to be careful with contrast doses, and movement is a big problem."
An ongoing study that his group started in early 2014 -- the Manchester Academic Health Sciences Center-funded SANTA trial -- epitomizes the problem. This is a phase II exploratory study looking at the use of the drug simvastatin in children with neurofibromatosis type 1 (NF1) and autism spectrum disorder. The purpose of this study is to test acceptability of involvement for families and the feasibility of imaging young children with NF1 autism.
The team has developed an acclimatization process that allows scanning without sedation or general anesthetic. They provide a CD with the scan noise, and have an associated social story, and importantly they work very closely with the play therapist team until the children feel comfortable. The work is beginning to yield some encouraging findings, but it is too early to comment on results, or draw conclusions, Stivaros said.