Wide variations exist in the indication, methodology, and frequency of CT usage not only within the same country but also between nations and continents, even though peer-reviewed guidelines are easily accessible, a new commentary in European Radiology has stated.
"These differences are caused by some objective factors like the number, type, and age of the locally available scanners on the one hand and numerous subjective factors on the other hand," wrote Prof. Zsolt Szücs-Farkas, PhD, consulting radiologist and head of department at Hospital Centre of Biel, Biel/Bienne, and Inselspital, Bern University Hospital, Switzerland.
Outdated or missing internal guidelines, the personal preferences of local radiologists and clinicians regarding image quality or specific phases after contrast media administration, suboptimal training of staff, or simply a low level of interest may all contribute to unnecessary high radiation and iodine dose, he added.
"Continuous education of both radiologists and technicians and regular revision of the CT regimens are essential. The key is probably having the personal interest to introduce and survey such improvements in the radiology department," Szücs-Farkas pointed out, noting that more than 400 million CT exams are performed worldwide per year, with an annual increase of around 3%-4%.
It is not necessary to possess a photon-counting CT or the latest AI to achieve good image quality at reasonably low radiation and contrast media dose in daily clinical routine, but everyone should know their own CT scanners and exploit all possibilities to achieve this goal, he continued.
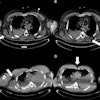
Radiation exposure is influenced by tailoring CT technical parameters to the patient rather than by patient size or scanner type. To reduce dose, CT vendors have implemented powerful tools like automated exposure control, beam-shaping filters, collimators, high-sensitivity x-ray detectors, and iterative image reconstruction, which are important ingredients of most modern scanners now.
Parallel to this, extensive research work has been done by the radiology community on testing these tools, as well as on other dose reduction techniques like low tube kilovoltage for CT exams using iodinated contrast media, especially for CT angiography (CTA) or the reduced number of CT phases, he noted. Other experimental and clinical studies have been directed at finding the optimal iodine concentration in organs and establishing the best contrast media administration protocols for different clinical tasks.
Global survey on CT use
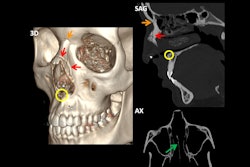
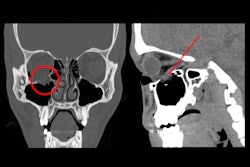
Szücs-Farkas wrote his commentary in response to an article published on 24 August 2024 by European Radiology, in which Dr. Lina Karout and colleagues at Massachusetts General Hospital presented the results of an international survey on CT use in three body regions (head, chest, and abdomen- pelvis) in 43 institutions of 16 countries on five continents. They set out to find differences in contrast media and radiation dose and to prove the findings from experimental papers suggesting higher radiation exposure from CT series after contrast media injection compared with native scans.
The authors found that the total iodine load with patient weight-based injection protocols was higher, lower, or equal to that with fixed injection rates, Szücs-Farkas explained. "Whether or not a high iodine load is advantageous depends vastly on body weight or diameter and the applied CT tube voltage, as the same total iodine load can be unnecessarily high in slim patients at 90 kVp or too low in obese subjects at 120 to 140 kVp for abdominal and liver scans," he wrote, adding that objective and subjective image quality were not analyzed, so no conclusion can be drawn on the possible beneficial effect of higher administered iodine amount.
With respect to the iodine delivery rate, head and chest CTA with weight-based protocols presented higher rates than fixed injection protocols, and this follows current guidelines as a high iodine delivery rate, at least to some degree, is beneficial for CTA, he continued. For routine head CT, sites using fixed injection protocols applied more CM at a lower rate compared with those using weight-based protocols, while the opposite was true for routine chest CT. Notably, nine to 10 of the 43 participating sites injected CM manually for nonangiographic CT exams and 3/43 obviously also for CTA, which possibly resulted in suboptimal image quality.
CT tube potential was relatively high as most institutions used 120 kVp or 140 kVp for the bulk of applications. Also, there was a lack of correlation between patient size and radiation dose. Before questioning the basic laws of medical physics, Karout et al pointed out inhomogeneities of their collected data and possible inadequate use of exposure control of the CT scanners by the sites.
The authors stress the need for translation of research results into daily practice and better education of staff worldwide. This is in line with recommendations of other recent studies demonstrating high variability within and across countries in their contrast media injection strategies and in the knowledge of contrast use among young radiologists and technicians.
According to Szücs-Farkas, "Even if there is probably not just one 'good' protocol to perform, e.g. a routine abdominal CT scan and differences in local preferences cannot be completely eliminated, survey results like those of Karout et al should initiate discussions in the institutions and can make a contribution to adapt internal CT protocols in order to converge towards established international recommendations."
You can read the full commentary here.