Ultralow-dose photon-counting CT is a promising tool for repeat follow-up exams in lung transplant patients, according to an Austrian study published on 10 September in Radiology.
The finding highlights the technique’s ability to reduce radiation doses in immunocompromised patients, noted lead author Dr. Ruxandra-Iulia Milos, of the Medical University of Vienna, and colleagues.
“To improve overall survival, patients with transplanted lung undergo many repeat CT examinations, which cumulatively are associated with a notable radiation exposure and may increase the risk of developing malignancy,” the group wrote.
Lung transplant is the last treatment option for many patients with end-stage lung diseases, yet their long-term survival is still limited due to the development of chronic lung allograft dysfunction and infections or malignancies from long-term immunosuppression, the authors explained. Currently, standard low-dose CT scans and chest x-rays are the preferred imaging methods for surveilling these patients.
Photon-counting CT is an emerging alternative technology. Yet, so far, data on its image quality when used with ultralow-dose (ULD) protocols are limited to cadaveric or phantom studies, the authors noted.
The researchers recruited 82 adult lung transplant recipients (median age, 64 years old) in a prospective trial from March 2023 to May 2023 at the Vienna Lung Transplantation Center. All participants underwent standard low-dose CT scans. Forty-one had ULD photon-counting CT scans that comparatively delivered 10% of the radiation dose and 41 had ULD photon-counting CT scans that delivered 20% of the dose.
Three readers with varying levels of experience viewed the subsequent 1-mm image reconstructions and subjectively rated them for image quality, the visibility of certain anatomic structures, and the presence of lung abnormalities.
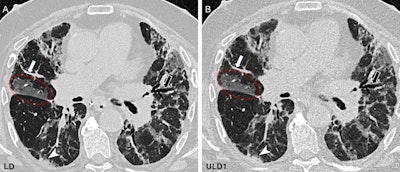 Chest CT in the craniocaudal direction at inspiration in a 62-year-old male participant with a combination of obstructive and restrictive chronic lung allograft dysfunction one year after lung transplant due to fibrosis. (A) Standard-of-care low-dose (LD) image (effective dose, 1.77 mSv) and (B) ultralow-dose (ULD1) image (effective dose, 0.307 mSv) show a comparison of image quality between protocols. Peripheral vessels (white arrows), bronchiectasis (black arrows), ground-glass opacity (red circles), and small consolidations (arrowheads) seen on the LD image (A) have excellent visualization on the ULD1 image (B), which was acquired with a target effective dose of approximately 20% of the LD protocol. The subjective image quality scores of the ULD1 image were 4, 4, and 3.Image and caption courtesy of the RSNA
Chest CT in the craniocaudal direction at inspiration in a 62-year-old male participant with a combination of obstructive and restrictive chronic lung allograft dysfunction one year after lung transplant due to fibrosis. (A) Standard-of-care low-dose (LD) image (effective dose, 1.77 mSv) and (B) ultralow-dose (ULD1) image (effective dose, 0.307 mSv) show a comparison of image quality between protocols. Peripheral vessels (white arrows), bronchiectasis (black arrows), ground-glass opacity (red circles), and small consolidations (arrowheads) seen on the LD image (A) have excellent visualization on the ULD1 image (B), which was acquired with a target effective dose of approximately 20% of the LD protocol. The subjective image quality scores of the ULD1 image were 4, 4, and 3.Image and caption courtesy of the RSNA
Key findings included the following:
- The ULD protocols yielded images of sufficient quality to adequately visualize anatomic structures in 33 of 41 participants (80.5%) to 41 of 41 participants (100%).
- The two ULD protocols yielded an approximately fivefold and tenfold reduction in radiation dose compared with standard low-dose CT.
- ULD PCT showed diagnostic accuracy greater than 70% for detecting most of the lung abnormalities, regardless of the reader’s experience in thoracic imaging.
“Ultralow-dose photon-counting CT yielded appropriate image quality to show anatomic structures and detect interstitial lung abnormalities, thus indicating its usefulness as a tool for long-term follow-up after lung transplant,” the authors wrote.
In an accompanying editorial, Dr. Pierluigi Ciet, of Erasmus MC-Sophia Children’s Hospital in Rotterdam, the Netherlands, suggested that the results are compelling.
“It is now clear that one of the most meaningful benefits of ULD PCT is indeed its ability to reduce radiation dose without compromising diagnostic capabilities,” he wrote.
As the technology continues to evolve, enhancements in image reconstruction algorithms, artificial intelligence integration, and noise reduction techniques could further improve its clinical utility, Ciet concluded.
The full study is available here.




















