
Incidental findings are the enemy, doing more does not always mean doing better, keep it simple, and don't be too afraid about renal failure with iodine: These are among the 10 golden rules of geriatric imaging written by an experienced German radiologist.
The concerns and the needs of the elderly can be easily overlooked in the daily work of a busy imaging department, according to Dr. Johannes Gossner, who is convinced that geriatric imaging requires a more personalized approach.
Gossner has worked as a radiologist at the Göttingen-Weende Hospital since 2009. This midsized hospital has a large geriatric department, and a special center for trauma surgery in the elderly ("Alterstraumazentrum") opened recently.
"What I learned in this time is how different the clinical status of elderly patients is. It is not uncommon for a 90-year-old patient to walk into the department and joke with the technicians, but there are also a large number of frail and severely ill bed-ridden patients," he told AuntMinnieEurope.com. "This difference is often not considered in decision-making about diagnostic imaging."
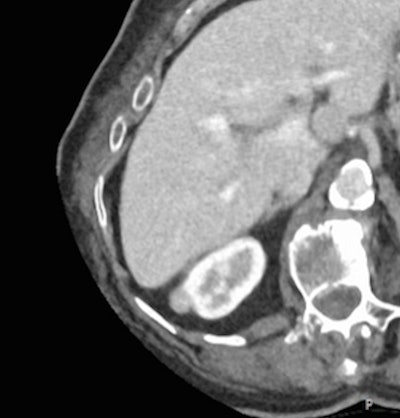 When an 81-year-old patient underwent CT for elevated liver markers, a small enhancing nodule (around 1 cm) on the right kidney was found incidentally. From the imaging appearance, this could be a small renal cell cancer. Given the low chance of metastasis of such a small renal cancer, a watchful-waiting approach with follow-up is reasonable. A biopsy or operation would represent an overtreatment for such a small lesion in an elderly patient. But in the case of a frail patient with limited life expectancy, even the need for follow-up imaging should be questioned. Image courtesy of Dr. Johannes Gossner.
When an 81-year-old patient underwent CT for elevated liver markers, a small enhancing nodule (around 1 cm) on the right kidney was found incidentally. From the imaging appearance, this could be a small renal cell cancer. Given the low chance of metastasis of such a small renal cancer, a watchful-waiting approach with follow-up is reasonable. A biopsy or operation would represent an overtreatment for such a small lesion in an elderly patient. But in the case of a frail patient with limited life expectancy, even the need for follow-up imaging should be questioned. Image courtesy of Dr. Johannes Gossner.Gossner's 10 commandments are listed in an article posted on 18 August by European Radiology, and they are summarized below:
1. Age is not a disease
Patients older than 70 years can be divided into patients with good health, vulnerable patients, and frail patients. Frailty is a syndrome with increased risk for poor health outcomes including risk of falls, incident disability, hospitalization, and mortality. Given the widely varying health status of elderly patients, it is crucial to tailor medical care individually.
2. Don't deny an examination because of advanced age only
Refusal of a radiological examination just because of age would be a clear case of ageism, but imaging of the frail elderly is time-consuming. An elderly and uncooperative patient needs a lot of time to undress, and positioning for the imaging procedure can be tough.
3. Doing more does not always mean doing better
For a moribund and dying patient, being transported around in a hospital, standing alone in attendance of an x-ray, and being carried on and off examination tables are stressful. Generally, if the test does not alter management, it should not be done, but imaging may be needed to get an overview of the patient state for clinical decision-making, even if a palliative approach is favored.
4. Keep it simple
MRI takes a lot of time and cooperation, and it can be stressful because of narrowness, noise, and long examination times. It should be used only if alternative imaging tests cannot answer the clinical question.
5. Radiation protection is not an issue in the elderly
Because of the presumed latency of stochastic radiation damage, taking at least 20 years, this is not an issue for the elderly.
6. Don't be too afraid about renal failure with iodine
Patients with an estimated glomerular filtration rate of more than 30 ml/min can safely receive iodinated contrast media. If iodinated contrast media is needed -- e.g., in patients with suspected pulmonary embolism or mesenteric ischemia -- it can be administered in almost every patient.
7. Don't fear gadolinium
Impaired renal function is also a risk factor for nephrogenic systemic fibrosis (NSF) after the use of gadolinium-based contrast agents (GBCA) in MRI. But, if contrast media is needed and a safe GBCA is chosen, the benefit clearly outweighs the small risk of NSF.
8. Incidental findings are the enemy
Around 30% of patients undergoing CT show one or more incidental findings. Even minor incidental findings may lead to further workup including further or follow-up imaging, endoscopy, or eventually tissue samples. In the frail elderly, only major incidental findings -- e.g., incidentally detected cancer, pulmonary embolism, or fractures -- should be worked up further.
9. Think about age-related changes
If there are minor imaging findings that do not explain the patient's symptoms (like minor fibrotic changes, slight brain atrophy, or ectasia of vessels), think about age-related changes. Unfortunately, only for brain imaging and osteoporosis, cutoff values or scores have been established for the differentiation between normal ageing and pathology.
10. Do no harm
The dilemma of overdiagnosis and subsequent overtherapy must be kept in mind at all times, and imaging should be used cautiously. In the care of the elderly, the guiding principle has to be "first do no harm."
Overall, the observable defensive style in medicine and the application of clinical guidelines often lead to a large number of radiological investigations, Gossner said. Many patients, especially the frail, report that they feel like they are forced to have further imaging exams, given the fast pace of clinical routine.
"Imaging, especially in the frail elderly, is a complex ethical task -- a fine line between ageism and over investigation, as Dr. Paul McCoubrie once wrote in AuntMinnieEurope.com," he noted. "Hopefully my editorial will encourage further reflections and discussions about this topic."




















