Only a third of women at high risk of breast cancer who have a provider recommendation for breast MRI actually undergo the examination, according a new investigation conducted in the U.S.
The results highlight the need to better encourage high-risk women to take advantage of this particular type of supplementary imaging, wrote a team led by Dr. Claire Conley of Georgetown University in Washington, DC.
"[Our study found that] high-risk women reported low uptake of screening breast MRI, indicating a gap in guideline-concordant care," the group noted in an article published on 28 August in Breast Cancer Research and Treatment. "Breast cancer knowledge and screening-supportive social norms are two key areas to target in future interventions."
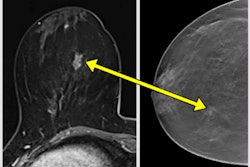
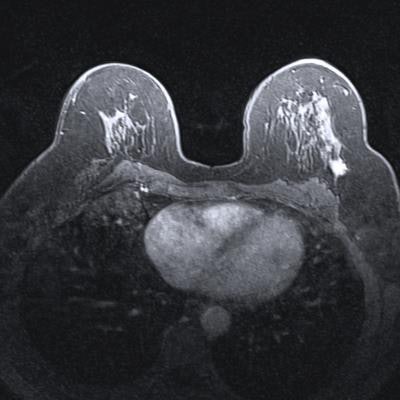
Professional organizations such as the American College of Radiology (ACR) recommend annual breast MRI for women at high risk of the disease (i.e., more than 20% lifetime risk). But breast MRI uptake among this population is underutilized, the researchers noted.
To better understand why, the group employed the Health Services Utilization Model (HSUM) to explore factors associated with use of screening breast MRI among high-risk women. This model assesses the use of health services by predisposing factors (race, age, and health beliefs), enabling factors (health insurance type, presence or lack of social support), and need factors (perceived risk of disease, screening-supportive social norms, and provider recommendation). The team also investigated factors such as a woman's knowledge of breast cancer, her perceived risk, and whether she had undergone screening breast MRI before.
Conley's group conducted a study that included data collected between August 2020 and January 2021 from 232 women at high risk of breast cancer. The team defined "high-risk" women as those having a genetic mutation or in a first-degree relative, a history of lobular carcinoma in situ, a history of thoracic radiation, or estimated lifetime risk of more than 20%.
Although half (51%) of the women had a recommendation for screening breast MRI from their healthcare provider, only a third (32%) had ever had the exam. The group also found that women's knowledge about breast cancer and screening-supportive social norms translated to a higher likelihood of them undergoing screening breast MRI (odds ratio, 1.15 and 2.21, respectively, with 1 as reference). No other Health Services Utilization Model variables were linked to a woman undergoing screening breast MRI, the authors reported.
"[Our study found that] high-risk women reported low uptake of screening breast MRI, indicating a gap in guideline-concordant care," they noted.
The findings underscore a need for more targeted interventions, according to Conley and colleagues. The researchers acknowledged that the study was conducted during the COVID-19 pandemic, and that the "generalizability of results is unclear."
"Breast cancer knowledge and screening-supportive social norms are two key areas to target in future interventions," they concluded. " Future studies with larger, more heterogeneous samples are needed to replicate these findings."
The complete study can be found here.