The disturbing case of an 80-year-old woman who developed compartment syndrome of the hand following a CT scan has focused attention on the range of adverse events that can result from the use of contrast agents in clinical practice.
The patient was admitted to hospital for investigation of syncopal episodes. A CT scan of the brain with contrast was ordered by the medical team for further analysis. While undergoing the scan, there was extravasation of contrast through the cannula in the dorsum of the right hand, authors from Monash University in Melbourne, Australia, explain in the May issue of the ANZ Journal of Surgery.
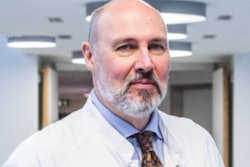
 Acute compartment syndrome developing on the dorsum of the right hand. Note discoloration and blistering of the skin on the dorsum of the hand. All images and captions courtesy of ANZ Journal of Surgery through Creative Commons Attribution 4.0 International License.
Acute compartment syndrome developing on the dorsum of the right hand. Note discoloration and blistering of the skin on the dorsum of the hand. All images and captions courtesy of ANZ Journal of Surgery through Creative Commons Attribution 4.0 International License.The woman had a past medical history of atrial fibrillation, for which she was anticoagulated with apixaban. Secondarily to the extravasation, a hematoma -- likely associated with the anticoagulant effect of apixaban -- also formed at the site of cannulation. In combination, these factors led to the development of acute compartment syndrome (ACS) of the hand.
"The patient was examined by the plastic surgery registrar on call, who noted the patient was in significant discomfort, the hand and fingers were pale and grossly swollen, and the skin on the dorsum of the hand was threatened," wrote Simon Savage, Carly Fox, and Stephen Goldie, PhD.
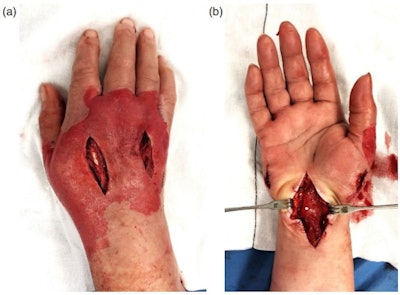 (A) Fasciotomy incisions to the dorsal compartments of the hand. (B) Fasciotomy incisions on the palmar aspect of the hand, demonstrating release of the thenar and hypothenar spaces as well as median nerve decompression through extended carpal tunnel release.
(A) Fasciotomy incisions to the dorsal compartments of the hand. (B) Fasciotomy incisions on the palmar aspect of the hand, demonstrating release of the thenar and hypothenar spaces as well as median nerve decompression through extended carpal tunnel release.The patient was rushed to the operating room, where evacuation of the contrast and hematoma was carried out under general anesthetic. Fasciotomies of the hand compartments and carpal tunnel decompression were performed.
Despite this intervention, the patient experienced extensive necrosis of the dorsal skin of her hand which subsequently required debridement and split skin grafting. At follow-up in clinic the skin grafts had healed, and the patients function improved slowly with hand therapy.
"Urgent surgical decompression of all affected compartments through fasciotomy is currently the gold standard of treatment for ACS. Initially, the patient should be closely monitored, any external compression such as a cast should be removed and the affected limb should be elevated above the level of the heart to balance the effort to maintain perfusion with the need to limit excessive swelling.
 (A) Dorsal right hand following debridement or dead skin and closure of fasciotomy wounds. (B) Dorsal right hand with split skin graft reconstruction.
(A) Dorsal right hand following debridement or dead skin and closure of fasciotomy wounds. (B) Dorsal right hand with split skin graft reconstruction.ACS is a rare condition that results from an increase in pressure in one of the body's closed fascial compartments, and this can lead to irreversible muscle and nerve damage due to a decrease in perfusion pressure and resultant ischemia, they continued.
ACS presents as paresthesia that may progress to anesthesia and paralysis as nerve ischemia worsens, and severe pain disproportionate to the causative procedure or trauma and pallor is present. It can be caused by acute fractures, as well crush injuries, burns, infections, and penetrating traumas, but it ultimately can be caused by anything that raises the pressure of a closed compartment.
Extravasation of contrast is a rare complication of contrast-enhanced CT scans, occurring in around 0.9% of patients and causing local reactions in approximately a quarter of these cases, according to the authors.
"Studies have identified contrast extravasation as a cause of ACS due to its direct mechanical compression of the region it enters," they noted. "While most extravasations cause mild discomfort, redness and swelling, the risk of more extensive tissue injury, ulceration and ACS is associated with a greater volume of extravasated fluid, with the use of hyperosmotic contrast and with the speed and route of injection."
Several methods have been suggested to decrease the frequency and harm of extravasation, including the use of nonionic, low osmolarity contrast, the supervision of contrast injecting pumps, the implementation of technologies that detect and notify of extravasation, and direction of the patient to report discomfort at the site of cannulation.
Efforts should be made to reduce the risk of extravasation where possible, the authors concluded. "Further research into the specific factors that increase the risk of harm from contrast infusion will provide better direction for future clinical practice."