
MRI is a valuable tool for assessing critical anatomical landmarks and features that determine the prognosis and management of rectal cancer patients, a leading research group reported at ECR 2023. The modality's also useful for tumor staging and restaging.
Dr. María Canedo Antelo and her colleagues from Santiago de Compostela University Hospital, A Coruña, Spain, are concerned that misleading anatomical, oncological, and surgical concepts -- assessable by imaging -- are influencing patient management in rectal cancer. They also fear the variability in the nomenclature between the different medical specialties involved in the multidisciplinary team is having an impact.
In an e-poster presentation that received a cum laude award at the Vienna congress, they aimed to uncover "the common misconceptions" about rectal cancer MRI.
"Colorectal cancer is the third most common malignant tumor worldwide. With advances in treatment and increasingly personalized patient management, the role of the multidisciplinary team is indisputable," the authors explained. "There is a need to clarify confusing concepts, which will define how imaging findings condition the management of these patients."
Clear definitions
Even the definition of "the rectum" is not without debate and varies according to medical speciality, they noted, although the most common definition is 15 cm from the anal verge.
The mesorectal fascia (MRF, visceral layer of the endopelvic fascia) encircles the rectum and the mesorectal fat, nodes, and lymphatic vessels to form a distinct anatomic unit: the mesorectum. The virtual space between the MRF and the parietal fascias is the "holy plane" that constitutes the theoretical surgical circumferential resection margin for total mesorectal excision (TME) or transanal TME, according to the authors.
Caudally, the MRF is in continuity with the intersphincteric plane; cranially, it is in continuity with the peritoneal reflection, they pointed out.
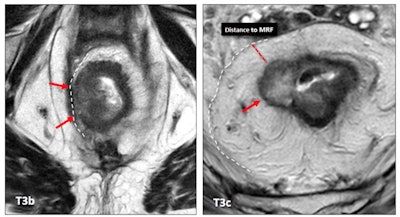 The treatment of a patient with rectal cancer mainly depends on the TNM (tumor, node, metastasis) stage and whether the mesorectal fascia (MRF) is involved. A T3b stage rectal tumor with MRF involvement (left, red arrows) compared to a T3c tumor with free MRF (right, red arrow). MRF involvement clearly worsens the prognosis of the tumor with a lower category of T staging. All images courtesy of Dr. María Canedo Antelo et al and presented at ECR 2023.
The treatment of a patient with rectal cancer mainly depends on the TNM (tumor, node, metastasis) stage and whether the mesorectal fascia (MRF) is involved. A T3b stage rectal tumor with MRF involvement (left, red arrows) compared to a T3c tumor with free MRF (right, red arrow). MRF involvement clearly worsens the prognosis of the tumor with a lower category of T staging. All images courtesy of Dr. María Canedo Antelo et al and presented at ECR 2023."MRF status is one of the most important risk factors for recurrence," they wrote. "A positive MRI-assessed margin between the tumor and MRF is defined as tumor lying within 1 mm of the MRF."
The MRF is a hypointense line on T2-weighted MRI, but it is a multilayered envelope that presents with gaps, and at some points it may not be visible on imaging. It is juxtaposed to the parietal fascias, which have different names according to location, they continued. Anteriorly, from the pelvic floor to the peritoneal reflection is the Denonvilliers' fascia; posteriorly, covering the sacrum, is the presacral fascia, which continues anteriorly as the pelvic parietal fascia.
T-staging makes a difference
MRI and endoscopic ultrasound tend to overstage early rectal tumors, Canedo Antelo and her colleagues stated. The degree of preservation of the submucosal layer seen on MRI as a hyperintense plane between the tumor and the muscularis propria (hypointense) should be assessed to recognize early tumors. Submucosal enhancing stripe status on contrast-enhanced MRI can serve as an independent predictor in the differentiation of stage T1 or lower rectal tumors from stage T2 tumors.
T3 category includes tumors with very different prognoses. Subdivision of T3 a/b and T3 c/d improves prognostic accuracy, they added.
"Differentiating T2 tumors from early T3 tumors can be difficult. A spiculated desmoplastic reaction in the perirectal fat or peritumoral inflammation may mimic tumor involvement. However, T2 and early T3 have the same prognosis," the authors wrote. "In peritonealized portions of the rectum (proximal), the tumor can be staged as T4a and does not represent carcinomatosis."
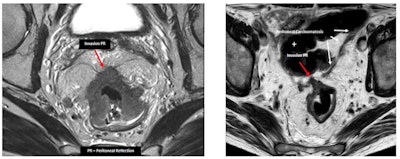 Serosal involvement does not necessarily represent peritoneal carcinomatosis. In peritonealized portions of the rectum (proximal), tumor can be staged as T4a and does not represent carcinomatosis. These tumors have a significantly higher risk of carcinomatosis (M1c stage). This group of patients might be eligible for new treatment strategies that aim to treat in an earlier or even preventive setting. (PR = peritoneal reflection)
Serosal involvement does not necessarily represent peritoneal carcinomatosis. In peritonealized portions of the rectum (proximal), tumor can be staged as T4a and does not represent carcinomatosis. These tumors have a significantly higher risk of carcinomatosis (M1c stage). This group of patients might be eligible for new treatment strategies that aim to treat in an earlier or even preventive setting. (PR = peritoneal reflection)In rectal cancer surgery, surgeons have to ligate the inferior mesenteric artery, and they can opt for a high or low ligation (preserving the left colic artery). A good description of the vascular anatomy brings safety to the surgery and can help the surgeon in his decision-making, they explained.
Recognizing mucinous tumors
The mucinous tumor has two distinct histologic subtypes: mucinous adenocarcinoma and signet-ring cell carcinoma. They are associated with young age, advanced tumor stage at presentation, higher rates of metastases, multiple metastatic sites, and a lower response to chemoradiotherapy.
"Mucinous tumors are defined histologically as those containing 50% or more of stromal mucin. They have a worse prognosis than similarly T-staged non-mucinous tumors," the authors noted. "It is incorrect to call a tumor that secretes a large amount of mucin into the lumen, 'mucinous.' "
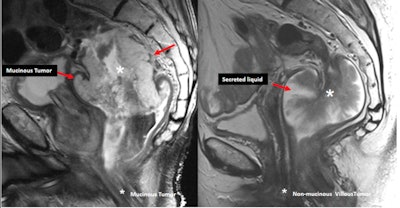 Mucinous tumors contain more than 50% of stromal mucin (left, sagittal T2-weighted MR image shows high signal intensity within the tumor). They must not be confused with non-mucinous lesions that secrete a large amount of liquid into the lumen (right).
Mucinous tumors contain more than 50% of stromal mucin (left, sagittal T2-weighted MR image shows high signal intensity within the tumor). They must not be confused with non-mucinous lesions that secrete a large amount of liquid into the lumen (right).Mucinous tumors typically show large areas of low attenuation and intratumoral calcification on CT and high signal intensity on T2-weighted MR images due to the presence of mucin pools. High signal intensity is defined as intensity similar to, or brighter than, the mesorectal fat. T2-weighted sequences with fat suppression, diffusion-weighted imaging (DWI) b0, or a dynamic contrast-enhanced series are helpful for diagnosis, they added.
Tumor response can be heterogeneous even within the same tumor, they continued. There are three main patterns of tumor response: shrinkage, fragmentation, and mucin production. Tumor response does not always result in downstaging.
Different tumor regression grading systems have been proposed, but they have limitations. Overall, DWI improves MRI tumor response assessment, they stated.
The co-authors of the ECR e-poster were Dr. Aldara Naveiras Calvo, Dr. Martin Bravo Gonzalez, Sandra Baleato Gonzalez, and Dr. Roberto Garcia Figueiras. To view the whole ECR 2023 poster, go to the EPOS section of the congress organizers' website.



















