Skipping radiotherapy may be an option for older women with early-stage breast cancer, suggest findings published on 16 February in the New England Journal of Medicine.
Researchers led by Dr. Ian Kunkler from the University of Edinburgh in Scotland found that while omitting radiotherapy was tied to increased incidence of local recurrence, doing so did not increase the incidence of distant recurrence as the first event post-treatment. It also did not significantly affect overall survival among women ages 65 or older who have low-risk, hormone receptor-positive early breast cancer.
"[Clinicians] may wish to discuss omission of radiotherapy as a treatment option for patients meeting the eligibility of the PRIME II trial," Kunkler told AuntMinnieEurope.com.
Over one in four breast cancer diagnoses in the U.S. are in women aged 65 to 74 years, and the incidence is rising, research indicates. Yet previous studies have shown that radiotherapy after breast-conserving surgery in older patients has a modest benefit when it comes to extending breast cancer survival.
Five-year results of the PRIME II trial -- which evaluated the impact of skipping postoperative radiotherapy in women 65 years of age or older with hormone receptor-positive breast cancer -- showed that radiotherapy was tied to a lower but "modest" percentage of patients having local breast cancer recurrence. These women had HR-positive T1 or T2 primary tumors and no lymph-node involvement and were treated with breast-conserving therapy and adjuvant endocrine therapy.
While some guidelines support not using radiotherapy in certain women ages 70 or older, radiotherapy is still commonly used in the U.S. in this population. Kunkler and colleagues wanted to report the 10-year outcomes of the PRIME II trial.
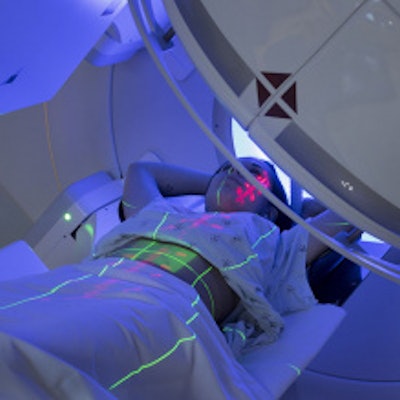
They looked at data from 1,326 women. Out of these, 658 were randomly assigned to receive whole-breast irradiation (40 to 50 gY) and 668 received no irradiation. The women were 65 years of age or older and had hormone receptor-positive, node-negative, T1 or T2 primary breast cancer. These were treated via breast-conserving surgery with clear excision margins and adjuvant endocrine therapy. Median follow-up was 9.1 years.
The researchers found a significantly higher cumulative incidence of local breast recurrence within 10 years between the two groups (p < 0.001), with a hazard ratio of 10.4 (with 1 as reference). However, this was not the case for distant recurrence as the first event. For reference, the 9.5% cumulative incidence in the no-radiotherapy group lies within range from the European Society of Mastology (EUSOMA) guidelines, which cites a maximum rate of local regional recurrence of 10% at 10 years.
| 10-year breast cancer recurrence results among radiotherapy, no-radiotherapy groups | ||
| Type of recurrence | Radiotherapy | No radiotherapy |
| Local recurrence | 0.9% | 9.5% |
| Distant recurrence as the first event | 3% | 1.6% |
The researchers also found that overall survival at 10 years was "almost identical" in the two groups: 80.8% in the no-radiotherapy group and 80.7% in the women who received radiotherapy. In fact, women in either group were more likely to die from other causes than from breast cancer. Of the 231 deaths that occurred in the study population, 31 (13%) were due to breast cancer.
"Patients and clinicians can balance the harms and benefits of irradiation knowing that avoiding it does not increase the risk of death from breast cancer," the team concluded.
Kunkler said the researchers are collaborating with other teams in Sweden and Canada on validating molecular signatures of breast cancer radiosensitivity in a historical Scottish Conservation trial of similar design to PRIME II.
"This should enable us to refine further selection of patients likely to respond to radiotherapy," he told AuntMinnieEurope.com.



















