The successful recognition of heterotopic pregnancy -- a rare complication, but one with the potential for significant morbidity and mortality -- begins with awareness of its imaging features and understanding of the diagnostic challenges, Australian researchers have reported.
Heterotopic pregnancy is defined as a condition that involves a simultaneous intrauterine and extrauterine pregnancy, and the prevalence ranges from 1:30000 in the general population to 1:100 in the context of assisted reproduction, explained Dr. Jeffrey Alexis, a radiology registrar at Gold Coast University Hospital, and Dr. Patricia Deonarine, a consultant radiologist at Qscan Radiology Clinics, both in Queensland.
"Anecdotally, in our institution, we have experienced an increasing incidence of heterotopic pregnancies with varying imaging and clinical presentations. This may be due to increasing use of assisted reproductive techniques, fertility or ovarian factors," they noted in a poster at the annual scientific meeting the Royal Australian and New Zealand College of Radiologists (RANZCR), held recently in Adelaide.
The diagnosis of heterotopic pregnancy can be challenging because the entity involves a normal intrauterine gestation, and there is a risk of missing the extrauterine pregnancy in the absence of a thorough understanding of the spectrum of heterotopic pregnancy imaging findings, the duo continued.
"The rarity of this entity can lead to reporter bias and result in a hesitancy to make the diagnosis," they stated. "Understanding of the key imaging findings would help to prevent a missed or overlooked diagnosis, which may lead to delay in treatment and further adverse sequelae."
A normal live intrauterine gestation should not preclude close examination of the adnexa, they added.
Early diagnosis and treatment is important to limit adverse outcomes. To highlight and raise awareness of the common imaging findings and diagnostic challenges of heterotopic pregnancy, Alexis and Deonarine presented details of two cases outlined below.
Case 1:
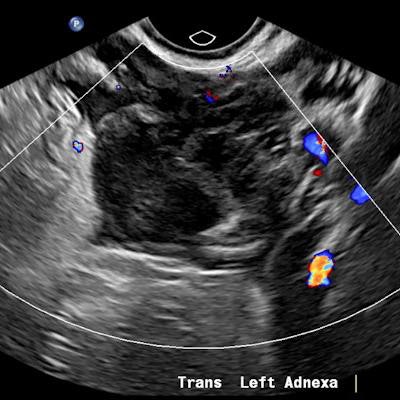
A 32-year-old female presented with severe constant left lower abdominal pain, per vaginal spotting and nausea. A pelvic ultrasound performed at six weeks' gestation demonstrated a viable intrauterine gestation and a small perigestational hematoma. A heterogeneous mass was noted abutting the left ovary. It featured peripheral vascularity, but no internal vascularity. There was small-volume pelvic free fluid with low-level internal echoes consistent with hemoperitoneum (see three images below).
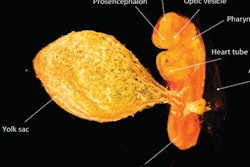
 Intrauterine gestational sac with fetal pole. All images courtesy of Dr. Jeffrey Alexis and Dr. Patricia Deonarine, presented at RANZCR ASM 2022.
Intrauterine gestational sac with fetal pole. All images courtesy of Dr. Jeffrey Alexis and Dr. Patricia Deonarine, presented at RANZCR ASM 2022. Left adnexal heterogeneous mass with an echogenic tubal ring sign (blue arrows) adjacent to the left ovary (red arrows).
Left adnexal heterogeneous mass with an echogenic tubal ring sign (blue arrows) adjacent to the left ovary (red arrows). Pelvic free fluid with low-level internal echoes consistent with hemoperitoneum.
Pelvic free fluid with low-level internal echoes consistent with hemoperitoneum.The patient was given a preliminary diagnosis of a hemorrhagic corpus luteal cyst. Heterotopic pregnancy was initially considered but thought less likely. The treating team opted for conservative management with a view to perform short-term follow-up ultrasound. Follow-up imaging two days later demonstrated a persistent left adnexal mass with interval increase in hemoperitoneum volume. The mass was seen to move separately to the left ovary on transvaginal/abdominal palpation maneuvers.
Diagnostic laparoscopy was performed on day 3 of presentation and heterotopic pregnancy was confirmed. A left salpingectomy was performed with preservation of the intrauterine pregnancy.
Case 2:
A 19-year-old female presented with suprapubic pain and a positive beta HCG. The initial ultrasound findings demonstrated both an intrauterine pregnancy and nonspecific adnexal mass. The intrauterine gestational sac featured both a gestational and yolk sac but no fetal pole. This correlated to an estimated gestational age of 5 weeks and 5 days. A heterogeneous left adnexal structure was demonstrated without internal vascularity. The left ovary was not readily identified. A hemoperitoneum was also present. The differential for the adnexal mass was thought to include a ruptured hemorrhagic cyst along with ovarian torsion and heterotopic pregnancy (see figures below).
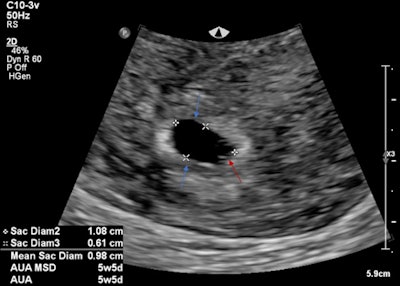 Intrauterine gestational sac (blue arrows) and yolk sac (red arrow). No fetal pole identified.
Intrauterine gestational sac (blue arrows) and yolk sac (red arrow). No fetal pole identified.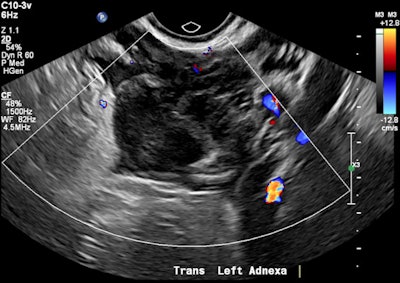 Avascular left adnexal heterogeneous mass.
Avascular left adnexal heterogeneous mass. Moderate free fluid with low level echoes within the pouch of Douglas consistent with hemoperitoneum.
Moderate free fluid with low level echoes within the pouch of Douglas consistent with hemoperitoneum.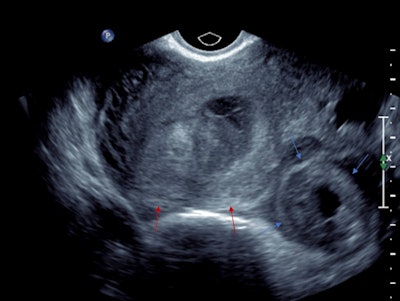 Transvaginal ultrasound in transverse orientation. The left adnexal mass demonstrates a hyperechoic tubal ring sign (blue arrows). The uterus (red arrows) demonstrates a double decidual reaction.
Transvaginal ultrasound in transverse orientation. The left adnexal mass demonstrates a hyperechoic tubal ring sign (blue arrows). The uterus (red arrows) demonstrates a double decidual reaction.The patient decided to have an outpatient surgical termination of the intrauterine pregnancy. A follow-up ultrasound was performed two days post termination due to increasing abdominal pain. A round, thick-walled avascular structure with a central hypoechoic component was seen within the left adnexa. It featured a hyperechoic rim consistent with a tubal ring sign. However, the left ovary was not identified. A moderate volume hemoperitoneum was also seen.
Diagnostic laparoscopy was performed, which confirmed a ruptured left tubal ectopic pregnancy with approximately 500 ml of hemoperitoneum and active bleeding. Left salpingectomy was performed and histological confirmation of products of conception was established.
Take-home messages
These two cases illustrate the concept of availability bias, which results from the clinician or radiologist's interaction with the rarity of a disease entity, according to the researchers.
"One fails to recognise the entities that are rare due to lack of recent experience or knowledge. Furthermore, satisfaction of search of the intrauterine pregnancy adds a further superimposed bias for the reporter and clinician with the temptation to ignore the adnexae," they noted. "These cognitive bias issues lead to a downplaying of the importance of a potential diagnosis or at worst missing the entity entirely."
Differentiating a hemorrhagic corpus luteal cyst from a tubal ectopic pregnancy can be challenging, and in early gestation the imaging features can be similar. A tubal ring sign and an adnexal mass that moves independently from the ovary are features highly suspicious for ectopic pregnancy. In addition, hemoperitoneum should raise further suspicion for alternative etiologies such as a complicated heterotopic pregnancy, they continued.
Deonarine, who is also a network training director at Gold Coast University Hospital, told AuntMinnieEurope.com that she is now developing a case review series on red flags and ectopic pregnancy. Her aim is to help to determine whether or not a pregnancy in an unknown location is ectopic. The project is still in the early stages, but she hopes to have something ready in 2023.