Dual-energy CT (DECT) lung perfusion scans can provide valuable complementary information to standard CT exams by depicting perfusion changes in systemic sclerosis patients with normal or minimally infiltrated lung parenchyma, researchers from Lille have reported.
"The introduction of DECT offers additional perspectives in the evaluation of systemic sclerosis-related pulmonary manifestations as it combines traditional cross-sectional imaging and creation of iodine maps," noted Antoine Dupont, Prof. Martine Remy-Jardin, and colleagues from the department of thoracic imaging at Hospital Calmette, University Hospital Center of Lille, in an article posted on 26 July by European Radiology.
Described as perfusion images, DECT scans measure iodine at a single time point and are currently considered adequate surrogate markers of lung perfusion. The technique has benefited from a decade of technological advances and is now mature enough to detect subtle perfusion defects as well as physiological gradients of lung perfusion, they stated.
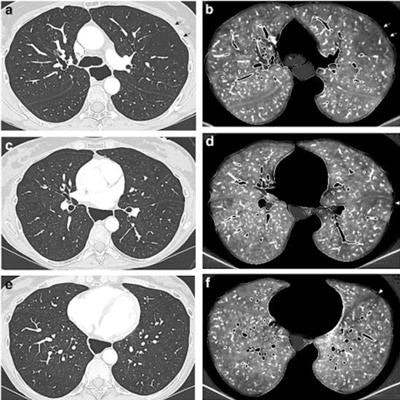
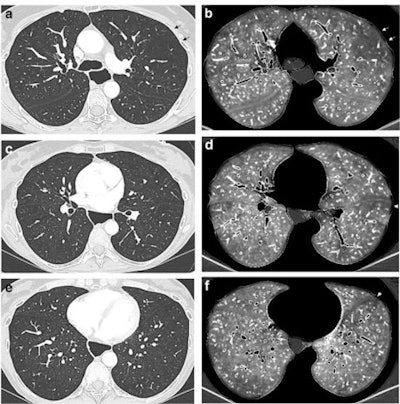 DECT angiographic exam obtained in a 55-year-old female nonsmoker with limited cutaneous systemic sclerosis diagnosed 24 years earlier (170 cm, 50 kg). Stable diffusing capacity of the lung alteration over two years. Paired lung and perfusion images obtained at the level of the upper (a, b), mid (c, d), and lower (e, f) lung zones. Absence of CT features of interstitial lung disease on lung images (a, c, e). Bilateral perfusion defects, combining patchy defects in both lungs (b, d, f), marked subpleural hypoperfusion in the lingula and left lower lobe (arrowhead; d, f) and a large triangular, pulmonary embolism-type perfusion defect (arrows; b) in the left upper lobe with reduced number of vascular sections in the corresponding lung image (arrows, a). No morphologic CT features of acute and/or chronic pulmonary embolism. Note the presence of marked esophageal dilatation. (All figures courtesy of Antoine Dupont, Prof. Martine Remy-Jardin and European Radiology).
DECT angiographic exam obtained in a 55-year-old female nonsmoker with limited cutaneous systemic sclerosis diagnosed 24 years earlier (170 cm, 50 kg). Stable diffusing capacity of the lung alteration over two years. Paired lung and perfusion images obtained at the level of the upper (a, b), mid (c, d), and lower (e, f) lung zones. Absence of CT features of interstitial lung disease on lung images (a, c, e). Bilateral perfusion defects, combining patchy defects in both lungs (b, d, f), marked subpleural hypoperfusion in the lingula and left lower lobe (arrowhead; d, f) and a large triangular, pulmonary embolism-type perfusion defect (arrows; b) in the left upper lobe with reduced number of vascular sections in the corresponding lung image (arrows, a). No morphologic CT features of acute and/or chronic pulmonary embolism. Note the presence of marked esophageal dilatation. (All figures courtesy of Antoine Dupont, Prof. Martine Remy-Jardin and European Radiology).Systemic sclerosis is an autoimmune connective tissue disorder that is characterized by a complex interplay of vascular abnormalities, immune system activation, and an uncontrolled fibrotic response. While the organ most commonly affected is the skin, systemic sclerosis is a systemic disease with the potential for multiple organ system involvement with special mention of the lungs and pulmonary vessels, recognized as a major cause of morbidity and mortality, the researchers wrote.
Interstitial lung disease is the most common pulmonary manifestation, affecting about 40% of patients. The identification and characterization of interstitial lung disease rely on high-resolution CT that can identify features suggestive of the histologic patterns of systemic sclerosis, for example, fibrotic or cellular nonspecific interstitial pneumonia and usual interstitial pneumonia, they continued.
CT is used to determine not only the pattern of lung injury but also its extent that can be combined with pulmonary function tests to predict interstitial lung disease progression, they explained.
Study logistics
The authors sought to evaluate lung perfusion in patients with systemic sclerosis and search for potential relationships between perfusion abnormalities and clinical, functional, and hemodynamic characteristics.
A total of 111 patients were recruited between January 2017 and December 2019. All patients underwent pulmonary function tests within two months of DECT.
Forced expiratory volume in one second and forced vital capacity were obtained by spirometry. Diffusing capacity of the lung (DLCO) was measured by single breath nitrogen tests. The percentage of predicted value for DLCO was corrected for measured hemoglobin. Fifteen patients had right heart catheterization-proven pulmonary hypertension.
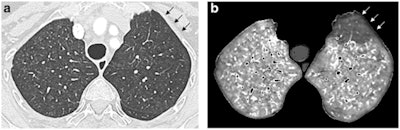 Dual-energy CT angiographic examination obtained in an 85-year-old female with limited cutaneous systemic sclerosis diagnosed 18 years earlier (159 cm, 60 kg), precapillary pulmonary hypertension recognized four years before this exam, and suspicion of pulmonary veno-occlusive disease or pulmonary capillary hemangiomatosis. Paired lung and perfusion images obtained at the level of the upper lobes (a, b), showing profuse, ill-defined lung micronodules in both lungs (a), highly suggestive of pulmonary veno-occlusive disease or pulmonary capillary hemangiomatosis, and a pulmonary embolism-type perfusion defect in the anterior segment of the left upper lobe (arrows, b). This perfusion defect was the only perfusion defect, seen in the absence of CT features of acute and/or chronic pulmonary embolism.
Dual-energy CT angiographic examination obtained in an 85-year-old female with limited cutaneous systemic sclerosis diagnosed 18 years earlier (159 cm, 60 kg), precapillary pulmonary hypertension recognized four years before this exam, and suspicion of pulmonary veno-occlusive disease or pulmonary capillary hemangiomatosis. Paired lung and perfusion images obtained at the level of the upper lobes (a, b), showing profuse, ill-defined lung micronodules in both lungs (a), highly suggestive of pulmonary veno-occlusive disease or pulmonary capillary hemangiomatosis, and a pulmonary embolism-type perfusion defect in the anterior segment of the left upper lobe (arrows, b). This perfusion defect was the only perfusion defect, seen in the absence of CT features of acute and/or chronic pulmonary embolism.The Lille team found that 37 patients had no systemic sclerosis-related lung involvement (group A). Another 56 patients had systemic sclerosis-related interstitial lung disease (group B) of variable extent (group B mild, ≤ 10% of lung parenchyma involved, n = 17; group B moderate: between 11% and 50%, n = 31; group B severe, > 50%, n = 8). Eight patients had pulmonary veno-occlusive disease or pulmonary capillary hemangiomatosis (group C).
Overall, lung perfusion was abnormal in 14 out of 54 patients (26%) with no or mild systemic sclerosis-related lung infiltration. It was abnormal in eight patients in group A (21.6%), 14 patients in group B (25%), and seven patients in group C (87.5%).
Patients with abnormal perfusion and no or mild systemic sclerosis-related lung infiltration had more severe scores of dyspnea and shorter walking distance than patients with similar lung findings and normal perfusion, suggesting the presence of small-vessel vasculopathy, the researchers pointed out.
The findings confirm the group's hypothesis that it's possible to detect changes at the level of pulmonary microcirculation on DECT lung perfusion images, despite the absence of lung parenchymal abnormality, Remy-Jardin told AuntMinnieEurope.com.
"DECT lung perfusion provides complementary information to standard CT images, both generated from the same data set," she explained. "We now plan to evaluate morphological changes over time in patients who had perfusion abnormalities in visually normal lung parenchyma."