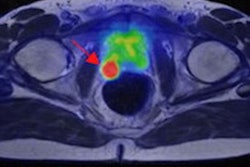
Prostate-specific membrane antigen (PSMA)-PET/CT imaging is comparable to MRI for detecting clinically significant prostate cancer. But MRI is still the more accurate modality for detecting the grade of disease, according to research presented on 3 July at the annual congress of the European Association of Urology (EAU) in Amsterdam.
The findings suggest that PSMA-PET/CT shows promise as an alternative for prostate cancer detection -- good news for patient care, wrote a team led by Dr. Lih-Ming Wong of St. Vincent's Hospital in Melbourne, Australia.
"This study confirms that the existing 'gold standard' of prebiopsy detection -- MRI -- is indeed a high benchmark," Wong said in a statement released by the society. "Even with fine-tuning, we suspect PSMA-PET/CT won't replace the MRI as the main method of prostate cancer detection. But it will likely have application in the future as an adjunct to the MRI, or for people for whom an MRI is unsuitable, or as a single combined 'diagnostic and staging' scan for appropriately selected patients."
The U.S. Food and Drug Administration (FDA) cleared the imaging agent gallium-68 (Ga-68) PSMA-11 for PSMA-PET/CT scans in 2020; a second agent, Pylarify, was cleared in 2021. Previous studies have suggested that PSMA-PET is a comparable tool to MRI for detecting clinically significant tumors in patients with prostate cancer.
Wong's group sought to investigate this theory further via a study that included 240 patients at risk of prostate cancer. Each underwent an MRI exam and a PSMA-PET/CT scan; if imaging indicated that prostate cancer was present, patients had a biopsy.
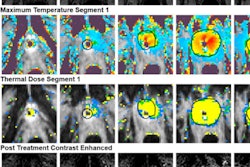
MRI found abnormalities suggestive of prostate cancer in 141 patients, and the PSMA-PET/CT scans found abnormalities in 198 patients. Of the 240 individuals who were included in the study, 181 (75%) underwent biopsy, and 82 of those were confirmed to have "clinically significant" prostate cancer, as defined by the relatively new International Society of Urologic Pathologists (ISUP) grading system for cancer severity.
Although PSMA-PET/CT imaging found more abnormalities than MRI exams did, MRI was more accurate in identifying the grade of prostate cancer than PSMA-PET/CT, at 75% compared with 62%, the team noted. But the two modalities were comparable when it came to identifying clinically significant prostate cancer, Wong noted.
"Our analysis found that MRI scans were better than PSMA-PET for detecting any grade of prostate cancer ... [but] when we looked only at clinically significant prostate cancers, there was no difference in accuracy," he said.
PSMA-PET/CT offers a good alternative to MRI for prostate cancer diagnosis, but more research is necessary, said Dr. Peter Albers of Heinrich-Heine-University Düsseldorf in Germany and chair of the EAU's chief scientific officer, in the statement.
"More research will be needed to explore the PSMA-PET/CT correlation between the standard uptake value and cancer aggressiveness, but the first steps down the road in finding the best diagnostic approach to clinically significant prostate cancer have been taken," he said.