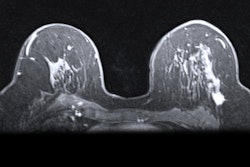
Telling radiologists in advance that there may be suspicious areas on mammograms may not improve their performance when interpreting the images, according to research published on 9 November in Radiology.
Radiologists who were told by radiographers about potentially cancerous areas on mammograms before they started reading had no statistically significant difference in cancer detection rates than radiologists who didn't get the warnings, according to a team led by Dr. Tanya Geertse from the Dutch Expert Centre for Screening in the Netherlands.
"Our study shows that it is not effective to expose radiologists to radiographers' warning signals during their initial interpretation of the screening mammograms," Geertse and colleagues said. "In general, radiologists are getting more and more signals or markers to support them in detecting lesions on medical images."
In the study, radiographers preread screening mammograms for possible abnormalities and relayed these warning signals to radiologists. The researchers said involving radiographers in this work increases their motivation and makes them more aware of the importance of producing high-quality mammograms. The practice is also intended to help reduce unnecessary recalls.
However, it is unknown when the best moment is to present these warning signals to radiologists.
Previous research suggests that the recall rate in the Netherlands is one of the lowest worldwide, but this has tradeoffs. Low recall rates may result in more missed subtle cancers, while high recall rates result in unnecessary follow-up, patient anxiety, and increased costs.
Therefore, Geertse et al wanted to find out the impact that the warning signals might have on early screening outcome measures when radiologists interpret mammograms.
In the study, radiologists were either blinded or nonblinded to warning signals. All discrepancies between radiologists and radiographers were reviewed during quality assurance sessions every six weeks, which may have led to secondary recalls. The study took place between September 2017 and May 2019.
Data from 10,9596 women with an average age of 62 were included in the study. Out of the total, 53,291 were in the blinded groups and 56,305 were in the nonblinded group.
| Impact of warning signals on radiologist mammogram interpretation | ||
| Nonblinded radiologists | Blinded radiologists | |
| Recall rate | 2.4% | 2.1% |
| Positive predictive value of recall | 26.2% | 30.6% |
| Cancers detected per 1,000 mammograms | 6.4 cancers | 6.5 cancers* |
The study authors wrote that radiologists should be blinded to warning signals from radiographers while interpreting screening mammograms, saying these signals could be presented immediately after interpretation to give radiologists the chance to change their recall decision.
"Additional cancers may be detected through review at quality assurance sessions," they added.
The team is planning to study additional views by radiographers and whether they prevent unnecessary recalls, as well as how a new procedure increases the performance of radiologists and affects quality assurance sessions.
In an accompanying editorial, Solveig Hofvind, PhD, from the University of Tromsø in Norway and Dr. Christoph Lee from the University of Washington wrote that one of the reasons for these results may be because of bias introduced in human interpretive processes for early warning signals.
They noted the Dutch screening program's warning system is "unique" and that computer-aided detection and artificial intelligence systems are designed to support or replace human radiologist interpretation.