
Direct communication between radiologists and patients resulted in a change in the radiological reports of 52 out of 122 cases (nearly 43%) in a new Swiss-Austrian study published online on 28 April in European Radiology.
 Dr. Andreas Gutzeit.
Dr. Andreas Gutzeit."Radiologists' communication can increase awareness among patients, which would significantly improve our own value from their perspective and our own political position. The fact that patients do not often notice us leads to a loss of perceived radiologist competence," said lead author Dr. Andreas Gutzeit, a radiologist at the Hirslanden Klinik St. Anna in Lucerne, Switzerland, and professor of radiology at ETH Zurich and the University of Salzburg.
"Doctor-patient communication can also improve the quality of our work. We are currently extremely dependent on information from the patient, the lack of which could lead to misdiagnosis and this was investigated in this study," he added.
With rising patient numbers and exams, there is a higher risk of information loss from a lack of radiologist-patient communication, causing error chains, and communication between radiologists and patients presents an opportunity to prevent this, Gutzeit noted.
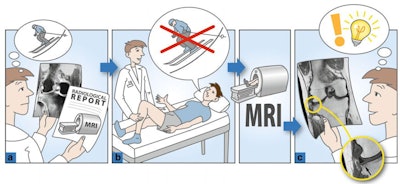 In this grade 3 change, the patient fell during skiing and now had left knee pain, according to the general practitioner. MRI showed pronounced high T2 signal in the lateral tibia, which was interpreted as post-traumatic edema following a skiing injury (a). After direct communication with the patient, the patient reported that he had never skied in his life and had never fallen. The pain would usually arise spontaneously at night (b). The authors retrospectively recognized a subchondral crescent sign in the tibia and interpreted the event as atraumatic osteonecrosis (c). A follow-up MRI three months later showed complete recovery of the subchondral bone fracture. All figures courtesy of Dr. Andreas Gutzeit and colleagues and European Radiology.
In this grade 3 change, the patient fell during skiing and now had left knee pain, according to the general practitioner. MRI showed pronounced high T2 signal in the lateral tibia, which was interpreted as post-traumatic edema following a skiing injury (a). After direct communication with the patient, the patient reported that he had never skied in his life and had never fallen. The pain would usually arise spontaneously at night (b). The authors retrospectively recognized a subchondral crescent sign in the tibia and interpreted the event as atraumatic osteonecrosis (c). A follow-up MRI three months later showed complete recovery of the subchondral bone fracture. All figures courtesy of Dr. Andreas Gutzeit and colleagues and European Radiology.The study prospectively included 122 consecutive outpatients undergoing MRI examinations at a single center between September 2019 and February 2020. Patients under 18 years of age or unwilling to talk to the radiologist after the exam were excluded. The technician team was consistent for all exams included in the study, and these were made on a 1.5-tesla and a 3T scanner.
Two radiologists drafted radiological reports in consensus using only the clinical information that was made available by the referring physicians. After this, one radiologist talked directly with the patient and recorded the duration of the conversation, which lasted an average of 170 seconds. The radiologists used the additional information from the patient to reevaluate the images in consensus.
They determined whether the radiological report changed due to the additional information and to what extent. The degree of change was graded on a 4-point Likert scale (1, nonrelevant findings, to 4, highly relevant findings), as outlined here:
- The patient provided information that was not clinically relevant to the diagnostic test. The addition of this information to the radiological report would be at the discretion of the radiologist.
- The patient provided information of limited clinical relevance. However, knowledge of this information would have improved the quality of the radiological report.
- The patient provided previously unknown information that can significantly alter the radiological/clinical diagnostic process, with a clear impact on the diagnosis or therapy/management.
- The patient provided information that would completely change the course of the clinical/radiological diagnostic process. The information provided by the patient shows that the radiological examination undertaken was of little value or completely wrong.
Striking results
Following direct communication, the radiologists changed the reports of 52 patients (42.6%). Of the 42.6% of cases in which the reports were changed, the alterations were highly relevant (grades 3 and 4) in 32.7%, indicating major changes with significant impact on patient management.
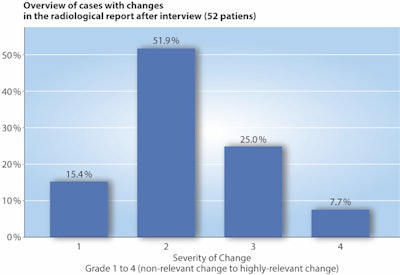
In more detail, of the 52 patients, the degree of change was classified as grade 1 for eight patients (15.4%), grade 2 for 27 patients (51.9%), grade 3 for 13 patients (25%), and grade 4 for four patients (7.7%). The reasons leading to changes were missing clinical information in 50 cases (96.2%) and the lack of additional external imaging in two cases (3.8%).
The authors noted that in 13 patients (25%), direct patient communication led to a highly relevant change in the report (grade 3) and in four patients (7.7%), misleading clinical information from the referring clinician could have led to the wrong diagnostic test or diagnosis (grade 4).
They also pointed to some study limitations; it was a single-center study with a limited number of study subjects and only one of the two radiologists performed the interviews. In addition, the team did not follow up most of the patients and therefore do not know to what extent any changes in the report might have impacted the treatments and outcomes of the patients.
However, with 7.7% of patients scoring 4 for diagnostic changes brought about by direct contact, should protocols on patient communication be changed? Gutzeit is cautious and believes that the latest study is just the beginning, and he pointed to several more underway at his institution that will further develop the topic.
AI vs. humans
AI and teleradiology will develop massive changes in radiology in the next few years, and radiologists should present themselves more as visible doctors who are interested in managing patients with optimal care, Gutzeit told AuntMinnieEurope.com.
"If we work in the background like machines we could really be replaced by machines in the future," he said. "Radiologists should be aware that imaging diagnoses are not purely rational findings but should always be interpreted in a clinical context. If we don't do that, AI will make similar findings to us in the future with the same failures. The solution has to be that we can be better than any machine through intelligent clinically orientated thinking and direct patient care."
To do this, radiologists need to get closer to the patient and, most importantly, expect that clinical indications may have errors or flaws that can lead to misinterpretation. Wrong diagnoses may be due to incorrect clinical assessments and examination orders, he noted. Therefore, clinical colleagues need to be concerned about their own evaluation quality and imaging requests.
Furthermore, teleradiology reports produce significantly higher false findings than onsite radiologists, according to larger studies, and this has never been explained, Gutzeit noted, adding that he believed these errors are due to the fact that teleradiologists are only dependent on the information provided by the clinician and can neither ask the patient nor the referring physician in case of ambiguities.
"In our view, these error rates need to be discussed and questioned further among the radiological community. AI will certainly not help us with these problems," he said.



















