The potentially devastating effects of multiple sclerosis (MS) on a person's central nervous system make it all the more paramount that clinicians use the most effective MRI sequences to diagnose suspected cases of the disease, a leading expert told ECR 2021 on Thursday.
In particular, 3D fluid-attenuated inversion recovery (FLAIR), T2-weighted MRI, and contrast-enhanced MRI are among the best tools to definitively determine the presence of MS and to evaluate patients' response to drug treatments.
"MRI is crucial for the diagnosis of MS," said Prof. Dr. Frederik Barkhof, PhD, professor of radiology, nuclear medicine, and brain imaging at Amsterdam University Medical Center. "As we are trying to make this more efficient in the next iteration of MR imaging criteria, even more emphasis is put on FLAIR, especially 3D FLAIR, which is my favorite sequence for many protocols including epilepsy and a series of other indications."
Multiple sclerosis lesions can appear anywhere in the central nervous system. As such, a definitive diagnosis of MS relies heavily on clinical observation by virtue of MRI and by identifying MS symptoms as they develop over time. Clinicians also need to look for lesions in other areas, such as the brain stem, cerebellum, ventricles, and cortical and intracortical regions.
"If we find lesions in two of these locations, we are in principle bound to make the diagnosis of MS," Barkhof told ECR 2021 virtual attendees.
The MR imaging sequences currently recommended to clinicians for MS are proton-density, T2-weighted, and 3D FLAIR in multiple planes, and, as needed, the accompaniment of a gadolinium-based contrast agent (GBCA). Given the promise of today's MRI hardware, images of MS can be acquired on most scanners in approximately five minutes, highlighted by isotropic resolution that allows for "reslicing" in multiple directions in approximately five minutes as well. Barkhof recommended T2-weighted imaging with gadolinium for an initial MRI MS scan and perhaps when the patient's treatment is changed.
If an MS patient does receive gadolinium, clinicians must be sure to wait five to 10 minutes between the injection and the scan. "This is most efficiently done by giving gadolinium at the beginning of the examination, then do your T2-weighted imaging and FLAIR, followed by T1-weighted imaging as the last sequence," he added.
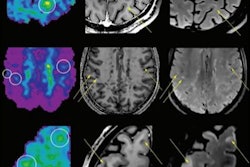
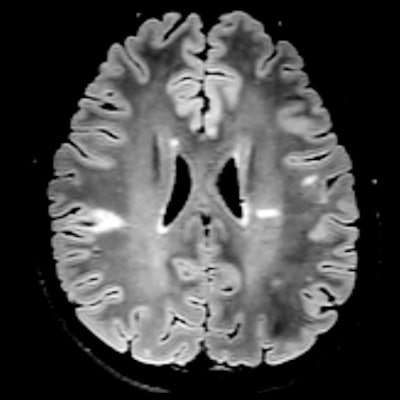
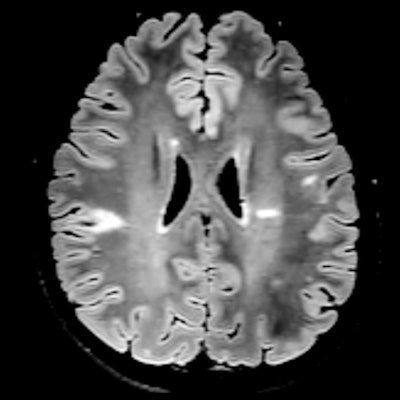 Axial FLAIR image shows hyperintense MS lesions in the periventricular and juxtacortical regions signifying dissemination in space. Image courtesy of Prof. Dr. Frederik Barkhof.
Axial FLAIR image shows hyperintense MS lesions in the periventricular and juxtacortical regions signifying dissemination in space. Image courtesy of Prof. Dr. Frederik Barkhof.Naturally, the best time to scan MS patients is at the time of diagnosis, using gadolinium to target the spinal cord with the appropriate MR imaging technique. Barkhof's preference is proton-density and T2-weighted imaging.
"With T2-weighted imaging, you can nicely see the spinal cord and the lesions, and with proton density you can see [lesions] even better, but it may be more difficult to see where the spinal cord is," he said.
Other MRI sequencing combinations work equally well, depending on the type of MRI scanner. In some situations, short-tau inversion recovery (STIR) can be advantageous, as can phase-sensitive inversion recovery (PSIR) and proton density with STIR.
Radiologists also should consider acquiring new baseline images for patients three to six months after their initial MRI scan. Once a definitive MS diagnosis is made, yearly MR imaging is recommended for the first two to three years, which can be done without gadolinium.
Additional MRI scans should be performed at the start of therapy to create "a good stable baseline after about a year," Barkhof said, and then to see if any new lesions appear to ensure the efficacy of the treatment.
"Up to two lesions can be tolerated over a year's time, which could be called minimal evidence of disease or mostly no disease activity," he added.
Interestingly, Barkhof said that magnet strength "does not really make a difference if you examine a patient at 1.5 tesla or 3 tesla. The brain [images] tend to be better at 3 tesla, with the spinal cord [images] slightly better at 1.5 tesla. It equals out, so it is not mandatory to scan patients suspected of MS at 3 tesla."
Of course, it is prudent to monitor for any side effects of MS drug therapy, especially progressive multifocal leukoencephalopathy (PML). The rare condition adversely affects the cells that produce the insulating sheath, known as the myelin, that wraps around nerves and the spinal cord.
In these circumstances, clinicians can use an abbreviated MRI protocol with 3D FLAIR, DWI, or T2-weighted imaging to screen for any signs or indications of PML in less than 10 minutes.