Women with high-risk breast tumors had more than double the chance of distant cancer spread if their cancer was interval detected rather than found on screening mammography, according to research presented on October 3 at the 2020 European Breast Cancer Conference.
Researchers know that interval breast cancers are particularly deadly, often because they frequently have higher-risk pathology than screen-detected cancers. But the new study shows that biology alone doesn't fully explain the difference in outcomes between interval-detected and screen-detected cancers.
In the new study, women with similar tumor genetics still fared better if their cancer was detected at screening. The findings demonstrate that the method of detection should be considered when planning treatment, according to presenter Dr. Josephine Lopes Cardozo, a doctoral candidate at the Netherlands Cancer Institute and a medical fellow at the European Organization for Research and Treatment.
"Although these tumors have the same biology -- all 70-gene, high-risk, and with similar tumor characteristics -- they have different prognoses based on their method of detection," Lopes Cardozo said in a press release. "This suggests that the method of detection is an additional prognostic factor in this group of patients."
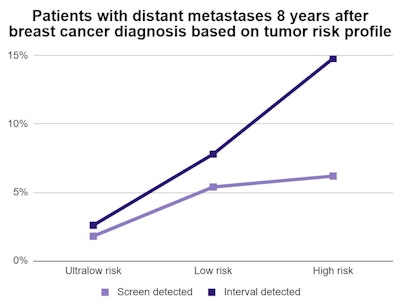
In their study of 1,102 patients with breast cancer in the Netherlands, Lopes Cardozo and colleagues found women with high-risk tumors had a 2.4-times higher risk of developing distant metastases if their cancer was identified in between screening mammograms. Nearly 15% of women with high-risk, interval-detected cancers had distant spread eight years after diagnosis, compared with 6% of women with high-risk, screen-detected cancers.
The findings were similar but not quite as stark for women with low-risk and ultralow-risk tumor types. The researchers found a 2.5% difference in distant spread among low-risk women with screen-detected and interval-detected cancer. That difference was less than 1% for women with ultralow-risk tumors.
| Type of breast cancer treatment based on method of detection | ||
| Treatment type | Screen detected | Interval detected |
| No adjuvant therapy | 36% | 17% |
| Endocrine therapy | 33% | 35% |
| Chemotherapy | 30% | 47% |
The type of treatment also differed based on method of detection. A higher percentage of women with interval-detected cancer underwent systemic adjuvant therapies, including chemotherapy and endocrine treatment, than those with screen-detected cancer.
"Most patients who received no adjuvant systemic therapy had grade I tumors, smaller than 2 cm, had no signs of cancer in their lymph nodes, and were classified as ultra-low or low risk by the 70-gene signature," stated Lopes Cardozo.
The findings were based on screening data from 1,102 women with breast cancer who participated in the Dutch national screening program. The program provides mammography screening every two years to women aged 50-75 in the country.
The international research team followed the patients for an average of 8.3 years, evaluating the length of time women were free of distant metastases based on tumor biology. Tumor risk and genetic profile were calculated using the MammaPrint 70-gene signature test.
Based on the findings, Lopes Cardozo said clinicians should look at both genetic signature and method of detection to optimize treatment plans for patients with both high- and low-risk tumor types.
"The method of detection combined with the 70-gene signature can further optimize treatment for patients at high risk of recurrence," she stated. "For patients with a very low risk of recurrence, longer follow-up may also help to identify those who are currently at risk of benign overtreated."



















