The COVID-19 pandemic is having a negative effect on breast cancer care, according to a panel held on 3 October at the 2020 European Breast Cancer Conference (EBCC). Three researchers presented evidence that the pandemic is tied to less breast screening, more loneliness, and fewer quality-of-life-enhancing procedures.
During the panel, EBCC presenters shared research that tried to quantify the effects of COVID-19 on breast cancer care.
The new research suggests the COVID-19 pandemic is affecting the entire continuum of breast cancer care -- but it also indicates that clinicians can take steps to mitigate some of the negative consequences. Below are three ways the pandemic is having an impact on breast cancer care in Europe:
1. Potentially more deaths due to missed screenings
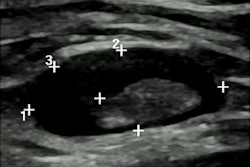
The halting of screening mammography during the pandemic could result in more women dying from breast cancer, according to a study from presenter Lindy Kregting, a doctoral student at the Erasmus MC University Medical Center Rotterdam in the Netherlands.
During her presentation, Kregting explained how her team used data from the Dutch Breast Cancer Screening Program to estimate the effects of four different strategies designed to make up for mammography appointments missed throughout 2020.
In April, the Dutch government halted its screening program, which provides mammography every two years to women ages 50-75. The program has since resumed screening mammography, but only at limited capacity.
All four scenarios modeled by the researchers resulted in an increase in breast cancer deaths per 100,000 women over the next 10 years.
The best-case scenario was a strategy that increased screening capacity in order to screen every woman who missed an appointment within six months of the initial delay. This scenario was linked to an increase of just 0.13 breast cancer deaths for every 100,000 women over the next 10 years --- but it is also the least realistic option, according to Kregting.
"We realize that most breast screening programs will not have the extra staff and equipment to do this," she stated.
Instead, the most practical way forward may be to resume breast screening as originally planned, while also temporarily raising the screening age, according to Kregting. This strategy would result in 1.85 more breast cancer deaths per 100,000 women over the next 10 years and could ensure women with delayed screenings get a final mammogram before aging out of the program.
2. Patients lonelier, less likely to seek care
Another study from the Netherlands found that the COVID-19 pandemic was affecting the mental health and willingness to get care of women with breast cancer.
A team led by presenter Dr. Claudio Bargon, a clinician and doctoral student at University Medical Center Utrecht, surveyed 1,051 women with breast cancer in Utrecht. Almost half of the respondents (48%) said they felt lonely during the pandemic.
Some patients also reported being less likely to seek help from their general physician (31%) or even their breast cancer physician (15%). Another 27% of respondents said they were worried about the effect the pandemic might have on their after care.
"This suggests that patients need reassurance that they should seek medical help when they need it and that we need to enable patients to access mental health support, even if this needs to be delivered online rather than face-to-face," Bargon stated.
3. Delays in quality-of-life procedures
A final study presented during the panel found women with breast cancer in Italy experienced delays in procedures that could boost their quality of life.
Presenter Dr. Alesandro Fancellu, an associate professor of surgery at the University of Sassari in Italy, and colleagues compared the experiences of breast cancer patients at their institution before and during the pandemic. The study included 41 women who received care in March of April of this year and 42 women treated during that same time period in 2019.
The women treated in 2020 were less likely to receive immediate breast reconstruction following mastectomy than those who underwent care one year prior. The cohort impacted by COVID-19 was also less likely to receive an intraoperative regional nerve block to reduce the likelihood of suffering from breast pain after surgery.
"These two procedures do not have an effect on the risk of breast cancer returning," stated Fancellu. "However, they do have an effect on women's quality of life following breast cancer surgery."
Fortunately, the team found no differences for the number of women who had surgery to treat breast cancer, how long they waited for surgery, or whether they underwent sentinel node biopsies to check for signs of lymph node spread. Facellu said the results show how clinicians can improve care if there's a second COVID-19 wave in Europe.
"We know that there could be a second peak of COVID-19 and, if that happens, we want to maintain the highest possible standards for our patients," he stated.