There is now a general absence of fear of COVID-19 patients among radiology staff, and the reduced anxiety levels have resulted in better patient handling, according to two chest radiologists with extensive experience of these cases.
"Initially staff were panicky and fearful upon hearing that a COVID-19 patient was to be examined. But now everyone is taking precautions and is sedate and calm," noted Dr. Abdul Haseeb Wani and Dr. Arshed Hussain Parry, both from Srinagar, the largest city and the summer capital of the Indian union territory of Jammu and Kashmir.
 Dr. Abdul Haseeb Wani (left) and Dr. Arshed Hussain Parry (right).
Dr. Abdul Haseeb Wani (left) and Dr. Arshed Hussain Parry (right).They added that nursing staff, radiographers, and radiologists have become much more aware of, and knowledgeable about, the various aspects of the disease. In their state and across India, the number of COVID-19 cases is growing, especially since lockdown was lifted.
"The mortality rate here remains very low, with 88 deaths reported so far among a total of 6,500 infected patients (approx. case fatality rate of 1.3%)," they told AuntMinnieEurope.com. "In view of low testing rates compared to developed nations, the actual case fatality rate may be even lower in our population. All the demised cases so far were mostly elderly and had an underlying co-morbid health condition."
Experiences of CT
Researchers from Srinagar have presented their experiences of CT in an article posted on 24 June by the European Journal of Radiology. Parry (first author) is a senior resident at the Sher-i-Kashmir Institute of Medical Sciences, and Wani (second and corresponding author) is consultant radiologist at the Government Medical College. Their key findings were the following:
- Two-thirds of the patients with laboratory-confirmed SARS-CoV-2 had a normal chest CT.
- One-third of patients with chest CT findings presented a typical pattern of ground-glass opacities in peripheral and posterior distribution.
- Small pulmonary vessel enlargement seems to be a unique feature of COVID-19 pneumonia with a diagnostic value.
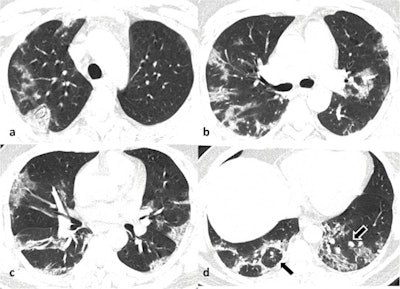 Noncontrast axial chest CT images in lung window settings of a 40-year-old male patient who tested positive for COVID-19, obtained eight days after symptom onset, in craniocaudal sequence (a,b,c,d) showing multiple patchy peripheral predominantly posterior ground-glass opacities with progression to consolidation in both lungs. There is also evidence of atoll sign in the right lung (black arrow in d) and perilesional vessel enlargement in the left lung (black arrow with white border in d). All images courtesy of Dr. Abdul Haseeb Wani, Dr. Arshed Hussain Parry, and the European Journal of Radiology.
Noncontrast axial chest CT images in lung window settings of a 40-year-old male patient who tested positive for COVID-19, obtained eight days after symptom onset, in craniocaudal sequence (a,b,c,d) showing multiple patchy peripheral predominantly posterior ground-glass opacities with progression to consolidation in both lungs. There is also evidence of atoll sign in the right lung (black arrow in d) and perilesional vessel enlargement in the left lung (black arrow with white border in d). All images courtesy of Dr. Abdul Haseeb Wani, Dr. Arshed Hussain Parry, and the European Journal of Radiology.In their study of 147 patients scanned between 17 March and 16 April 2020, 104 (71%) were men and 43 (29%) were women, and the mean age was 40.9 ± 17.2 years (range, 24-71 years).
Lung parenchymal abnormalities were seen in 51 (35%) cases, whereas 96 (65%) cases with a positive reverse transcription polymerase chain reaction (RT-PCR) result had a normal chest CT. Only 12% of patients were dyspneic, 6% had desaturation, 7% had increased respiratory rate and 11% had comorbidities. Among the patients with abnormal CT findings, bilateral 39/51 (76.5%), multilobar (88%) lung involvement with a predominant peripheral and posterior distribution was commonly observed.
Ground-glass opacity (GGO) was the dominant abnormality found in all 51 cases. Pure GGO was observed in 15 (29%), GGO with crazy-paving pattern was seen in 15 (29%), and GGO mixed with consolidation was noted in 21(41%). Perilesional or intralesional segmental or subsegmental pulmonary vessel enlargement was observed in 36 (71%) of cases.
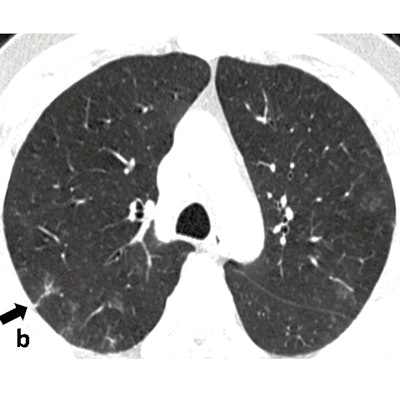
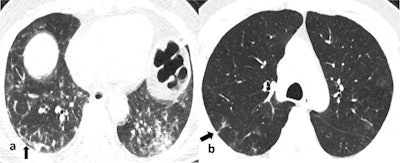 Noncontrast chest CT axial image (a) in a 62-year-old male patient who tested positive for COVID-19, obtained nine days after symptom onset, showing subpleural curvilinear lines (black arrow) with multiple reticulations in the right lower lobe and mixed ground-glass opacities and consolidation pattern in the left lower lobe. Noncontrast chest CT axial image (b) in a different 61-year-old male patient who was COVID-19 positive, obtained six days after symptom onset, shows evidence of subpleural reticulations (black arrow) in the posterior segment of the right upper lobe with a few rounded morphology ground-glass opacities in the left upper lobe.
Noncontrast chest CT axial image (a) in a 62-year-old male patient who tested positive for COVID-19, obtained nine days after symptom onset, showing subpleural curvilinear lines (black arrow) with multiple reticulations in the right lower lobe and mixed ground-glass opacities and consolidation pattern in the left lower lobe. Noncontrast chest CT axial image (b) in a different 61-year-old male patient who was COVID-19 positive, obtained six days after symptom onset, shows evidence of subpleural reticulations (black arrow) in the posterior segment of the right upper lobe with a few rounded morphology ground-glass opacities in the left upper lobe."Most of the findings we observed were in tune with the published data, however, low prevalence of chest CT findings in our population was intriguing," they reported. "Secondly, segmental pulmonary vessel enlargement was a unique finding in COVID-19 pneumonia that we observed in our cohort. This finding is peculiar to COVID-19 pneumonia and has a diagnostic value."
Paradigm shift
Since mid-April, between 150 and 200 more CT exams have been performed at the hospital. Initially, noncontrast CT was the norm, but since pulmonary vascular complications are frequently reported in severe COVID-19 cases with a need for anticoagulation, CT pulmonary angiographies are now carried out in patients suspected of having underlying pulmonary embolism as the cause of respiratory deterioration.
"There has been a paradigm shift in the imaging strategy of COVID-19 patients in our hospital," commented Wani and Parry. "Initially when we were dealing with the COVID-19 outbreak, we were not familiar with the way the virus would behave in our population, so there was a tendency to do CT in all cases, including cases with mild symptoms. But our observations led us to a preliminary conclusion that CT findings may be absent, even in symptomatic cases."
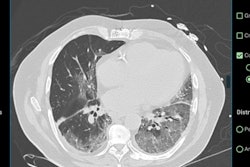
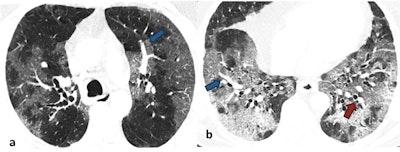 Noncontrast axial chest CT images in lung window settings of a 62-year-old male patient who tested positive for COVID-19, obtained five days after symptom onset, showing diffuse ground-glass opacities in peripheral and central distribution progressing to frank consolidation. There is also evidence of intralesional vessel enlargement (blue arrows in a & b) and bronchial dilatation (red arrow in b).
Noncontrast axial chest CT images in lung window settings of a 62-year-old male patient who tested positive for COVID-19, obtained five days after symptom onset, showing diffuse ground-glass opacities in peripheral and central distribution progressing to frank consolidation. There is also evidence of intralesional vessel enlargement (blue arrows in a & b) and bronchial dilatation (red arrow in b).They realized that CT cannot be used a screening modality in COVID-19 in lieu of RT-PCR, so CT is performed only in patients who are severely ill or show respiratory worsening during the hospital stay.
Infection control and PPE
To reduce the chances of cross-infection in the radiology department, every patient is transported to the CT suite wearing a mask. Two radiographers are involved in performing the CT: One sets up the patient on the CT gantry, while the other controls the console room. Both wear personal protective equipment (PPE) consisting of a cap, goggles or a face visor, N95 respirator, waterproof gown (GSM 90), plastic shoe covers, and hand gloves.
The CT gantry is covered with a disposable sheet before positioning the patient on it. After performing the CT, the gantry is cleaned with 0.1% sodium hypochlorite solution or 70% alcohol. The floor of the CT suite is also cleaned every four hours with sodium hypochlorite solution. It usually takes 10 minutes to clean the room between patients. Passive air exchange of the CT suite is allowed for approximately 30 minutes before the next examination.
Looking to the future, the Srinagar team is now working on vascular complications in COVID-19 pneumonia. These are seen quite frequently in severe COVID-19 cases and contribute to mortality.
"We are trying to connect the three dots of imaging, histopathology, and clinical data to analyze the vascular complications of COVID-19," Wani and Parry elaborated. "We are trying to find out what additional therapeutic strategies need to be adopted to reduce the vascular complication related mortality in severe COVID-19. We are focusing on immunothrombosis as the underlying pathophysiological mechanism for high rates of vascular complications in COVID-19."