A group of expert radiologists and urologists have released a new set of recommendations on quality issues in prostate MRI, covering acquisition, reporting, training and education, and experience prerequisites.
The Delphi consensus paper was developed with the support of the European Society of Urogenital Radiology (ESUR) and the European Association of Urology's section of Urologic Imaging (ESUI), and it was published on 19 May as an open-access document in European Radiology.
"We think this is an important topic for the radiological community because prostate MRI is now used as upfront diagnostic tool in the recently changed prostate cancer guidelines," noted senior author Prof. Jelle Barentsz and joint first authors Dr. Maarten de Rooij and Dr. Bas Israël, from the departments of radiology and urology at the Radboud University Medical Center, Nijmegen, the Netherlands, in an email to AuntMinnieEurope.com. "We agreed on many things (74% of the 55 items) with quite a sizeable expert panel (44 radiologists and urologists)."
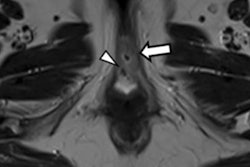
![T2-weighted image shows the prostate of a patient (age unknown) with an elevated prostate-specific antigen (PSA) level and previous negative transrectal ultrasound guided biopsies. Multiparametric MRI showed a large PI-RADS 5 lesion in the anterior part of the transition zone, which proved to be a clinically significant prostate cancer (International Society of Urologic Pathologists [ISUP] grade 3). Benign prostatic hypertrophy in the transition is visible as 'organized chaos' (blue area). All images courtesy of Prof. Jelle Barentsz, Dr. Maarten de Rooij, and Dr. Bas Israël.](https://img.auntminnieeurope.com/files/base/smg/all/image/2020/05/ame.2020_05_27_16_34_2157_2020_27_05_MRI_Insider_prostate_MRI_1.png?auto=format%2Ccompress&fit=max&q=70&w=400) T2-weighted image shows the prostate of a patient (age unknown) with an elevated prostate-specific antigen (PSA) level and previous negative transrectal ultrasound guided biopsies. Multiparametric MRI showed a large PI-RADS 5 lesion in the anterior part of the transition zone, which proved to be a clinically significant prostate cancer (International Society of Urologic Pathologists [ISUP] grade 3). Benign prostatic hypertrophy in the transition is visible as "organized chaos" (blue area). All images courtesy of Prof. Jelle Barentsz, Dr. Maarten de Rooij, and Dr. Bas Israël.
T2-weighted image shows the prostate of a patient (age unknown) with an elevated prostate-specific antigen (PSA) level and previous negative transrectal ultrasound guided biopsies. Multiparametric MRI showed a large PI-RADS 5 lesion in the anterior part of the transition zone, which proved to be a clinically significant prostate cancer (International Society of Urologic Pathologists [ISUP] grade 3). Benign prostatic hypertrophy in the transition is visible as "organized chaos" (blue area). All images courtesy of Prof. Jelle Barentsz, Dr. Maarten de Rooij, and Dr. Bas Israël.Suboptimal image acquisition and reporting results in clinicians losing confidence in the technique and returning to the non-MRI systematic biopsy pathway, so it's crucial to establish quality criteria for multiparametric MRI, they explained. Checking and reporting of image quality should be mandatory, and prostate radiologists must attend theoretical and hands-on courses, supervision sessions, and regular self- and external performance assessments.
Doing the groundwork
Before the new guidance was compiled, the 44 panelists completed two rounds of questionnaires comprising 55 items under three headings: image quality assessment, interpretation and reporting, and radiologists' experience plus training centers. Of the 55 questions, 31 were rated for agreement on a 9-point scale, and 24 were multiple-choice or open. To be categorized as an agreed item, there had to be agreement among at least 70% (score 7-9) of panelists and a disagreement rate of less than 15%. For the other questions, a consensus was considered to be more than 50% of votes.
The panelists achieved a consensus on 24 out of 31 of agreed items and 11 out of 16 of other questions. They agreed that reporting of image quality should be performed and implemented into clinical practice, radiologists should use self-performance tests with histopathology feedback and compare their interpretation with expert-reading and use external performance assessments, and radiologists must attend theoretical and hands-on courses before interpreting prostate MRI.
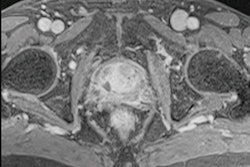
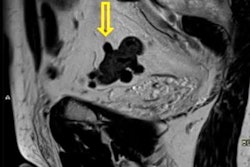
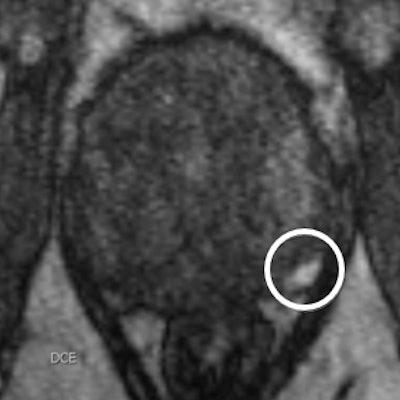
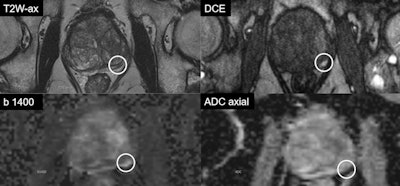 Multiparametric MRI of 74-year-old patient with a PSA of 9.6. Transperineal MR-guided biopsy showed an ISUP grade 4 cancer (Gleason score 4 + 4 = 8). The case highlights the benefit of using dynamic contrast-enhanced MRI (DCE). The small lesion in the left peripheral zone shows vivid focal enhancement on DCE. Such small lesions can easily be missed without DCE. The patient had a successful radical prostatectomy.
Multiparametric MRI of 74-year-old patient with a PSA of 9.6. Transperineal MR-guided biopsy showed an ISUP grade 4 cancer (Gleason score 4 + 4 = 8). The case highlights the benefit of using dynamic contrast-enhanced MRI (DCE). The small lesion in the left peripheral zone shows vivid focal enhancement on DCE. Such small lesions can easily be missed without DCE. The patient had a successful radical prostatectomy.There was no consensus, however, on outcomes statements of prostate MRI assessment as a quality marker.
"The distribution of the PI-RADS (Prostate Imaging Reporting and Data System) assessments as a measure of quality is difficult since it is highly dependent on the prevalence of high-grade prostate cancer (Gleason Grade Group ≥ 2) in the population," the authors pointed out. "For instance, this number depends on the region (geographical), the extent of the PSA screening, and previous (negative) biopsy sessions. Also, in the literature, the number of PI-RADS 3 lesions varies significantly between studies: range 6.4%-45.7%."
It seems likely that the percentage of PI-RADS 3 lesions in particular can be an essential measure of reader quality. This should be as low as possible, but it is understandable that no agreement was reached on an exact number, they added.
Training difficulties
The number of prostate MRI teaching courses in Europe is quite good, but the structure of the courses varies widely, and radiologists who have little or no experience of assessing prostate MRI should realize that training is essential, the authors continued.
"Prostate MRI is a difficult examination, with many nuances (multiparametric oncological diagnostics)," they told AuntMinnieEurope.com. "You can only learn these nuances if you follow good courses, gain sufficient experience, and your performance is actually tested. Interactive supervised education is rare, and education with double reads -- like a supervising radiologist does with his/her radiology-residents -- is exceptional."
National or European organizations have a key role to play in individual certification and accreditation of centers, but the details have yet to be determined. In general, the accuracy for detecting high-grade cancers improves with training, but very little research has been done into the precise effect of training on individual performance, according to the authors.
Impact of COVID-19
In Nijmegen, the number of prostate MRI examinations has declined sharply as a result of the COVID-19 pandemic, most probably because men are less likely to go to the doctor or specialist for fear of COVID-19 infection, noted Barentsz, de Rooij, and Israël.
"We had a temporary drop in prostate MRI exams of 50%, but we are now seeing a recovery to almost the pre-COVID-19 level," they said. "Looking at the Netherlands, we see a 30% reduction in the number of prostate cancer diagnoses. For other urogenital tumors, this has returned to 'normal'. However, prostate cancer is still lagging behind, possibly due to less patient-driven opportunistic PSA screening."
 The Nijmegen team: from left to right are Prof. Jelle Barentsz, Dr. Maarten de Rooij, and Dr. Bas Israël.
The Nijmegen team: from left to right are Prof. Jelle Barentsz, Dr. Maarten de Rooij, and Dr. Bas Israël.Looking to the future, the researchers' main goal is to make the recommendations in the consensus paper more specific. For instance, they are formulating the criteria for image quality assessment of prostate-MRI with Prostate MRI Quality Subcommittees of the ESUR and the ESUI. In addition, they are continuing to emphasize the importance of certification and accreditation with the national radiological societies.