In a direct comparison, FDG-PET proved superior to MRI with arterial spin labeling (ASL) for diagnosing and differentiating various forms of dementia; however, there remains a need for the latter modality, according to a Belgian study published online on 20 January in the European Journal of Nuclear Medicine and Molecular Imaging.
Two readers achieved higher sensitivity and greater diagnostic confidence using FDG-PET against MRI with enhanced multiplane tagging ASL (eASL), which is used to quantify cerebral blood perfusion. Yet, despite the differences, the researchers still believe MRI with eASL can play an important role in dementia diagnosis.
"Within the setting of this clinical study on subjects referred for suspicion of neurodegenerative dementia, the main finding was that F-18 FDG PET should still be seen as the primary choice, as it performed better compared with eASL in terms of sensitivity, reader confidence, and lower variability in key regions in dementia diagnosis," wrote lead author Jenny Ceccarini, PhD, and colleagues at University Hospitals Leuven.
"Moreover, eASL could be considered a potential alternative to F-18 FDG PET to assess neurodegeneration in patients with cognitive impairment when the latter is unavailable, or in case dual-parameter evaluation may still serve as complement to neuroreceptor or protein deposition PET studies when a single simultaneous investigation is performed," they noted.
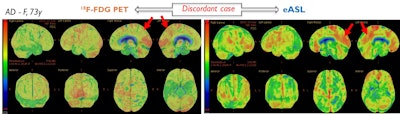
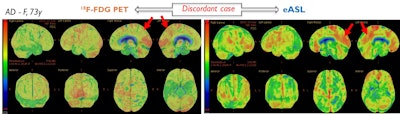
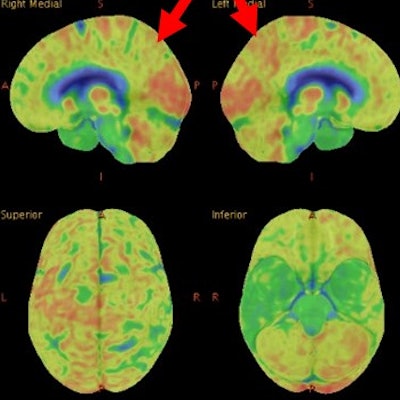
A discordant case of a patient with Alzheimer's disease (AD), correctly classified with FDG-PET based on hypometabolism in the left posterior cingulate gyrus (red arrow) extending to the precuneus, but wrongly diagnosed based on MRI-eASL perfusion. Images courtesy of Ceccarini et al.
Diagnosing dementia
PET with FDG and various other radiotracers has been used to attempt to diagnose the early onset of Alzheimer's and dementia. At the same time, perfusion MRI with ASL has been used to indirectly measure neuronal functioning, but its diagnostic value in clinical dementia diagnosis has not been determined, the researchers noted. They cited previous studies in which sensitivity ranged from 53% to 80% and specificity from 62% to 84%, "probably due to differences in ASL techniques, type of comparative analysis, and due to the heterogeneity of small cohorts."
Given that few PET/MRI studies have compared FDG-PET with MRI using ASL, Ceccarini and colleagues sought to conduct a head-to-head comparison between eASL and F-18 FDG PET in the clinical context of subjects who were referred for suspected neurodegenerative dementia, they added.
The prospective study included 27 patients (mean age, 64.3 ± 11.2 years ) referred for a brain scan between December 2016 and June 2017 due to recent cognitive decline and possible dementia. The routine, 20-minute PET/CT scan was performed 30 minutes after injection of 150.5 (± 11.5) MBq of F-18 FDG; this was followed immediately by a PET/MRI scan on a simultaneous 3-tesla system (Signa, GE Healthcare), which featured an eASL sequence.
The patients also underwent routine clinical, neurological, and neuropsychological exams, with some also undergoing structural MRI with T1-weighted and fluid-attenuated inversion recovery (FLAIR) sequences. In all, 14 patients had a neurodegenerative cognitive disorder -- Alzheimer's disease, Lewy body dementia, or frontotemporal dementia -- and 13 had no evidence of neurodegeneration.
In addition, the study included 30 healthy control subjects who were matched by age and gender to the patient cohort. The control subjects underwent a 60-minute PET/MR scan some 60 minutes after injection of 152.2 (± 11.1) MBq of F-18 FDG.
Seeing is believing
The two readers, who were blinded to the final diagnoses, evaluated the MRI-eASL and FDG-PET results by determining the presence and degree of dementia. The readers also rated their diagnostic confidence in using the two approaches on a scale of 1 to 4.
In the visual read of images to distinguish between normal results and neurodegeneration, the duo achieved a mean sensitivity of 93% with FDG-PET, compared with a significantly lower mean sensitivity of 64% with MRI-eASL (p = 0.03). Mean specificity was fairly consistent between the two modalities, with FDG-PET at 70% and MRI-eASL at 71%. Mean accuracy was 75% with FDG-PET, compared with 68% for MRI-eASL, but the difference was not statistically significant.
One reader diagnosed nine (64%) of the 14 patients with confirmed cases of dementia using FDG-PET, while the other reader accurately called eight (57%) of those patients. The pair had less success with MRI-eASL, correctly diagnosing seven (50%) and four patients (29%), respectively, with confirmed dementia.
Reader confidence
For several regions of the brain associated with dementia, the readers' diagnostic confidence waned with MRI-eASL. They were less confident in their conclusions when using eASL to rate blood flow, compared with FDG metabolism, in the temporal cortex, occipital cortex, striatum, and thalamus among all patients with a suspected diagnosis of dementia and among the entire control group.
Ceccarini and colleagues cited several factors that distinguish these results from previous research. First, the prospective study was conducted "in a true clinical context of patients with cognitive impairment referred for exclusion/confirmation of a neurodegenerative disorder after careful clinical and paraclinical workup," they wrote.
"Moreover, we included an age- and gender-matched healthy control set acquired on the same instrumentation that was evaluated in a blinded fashion and the heterogeneity of final diagnoses represents a true clinical scala of uncertain cases with cognitive impairment," the authors added.