It is a commonly held belief among radiologists that breast density has a key role in the breast cancer screening process. Studies show that women with very dense breasts are four to five times more likely to develop breast cancer than women with less dense breasts.1,2 Screening for cancer is especially important for women with dense breasts, yet unfortunately, it can also be particularly challenging. Underlying cancers can be masked by dense breast tissue on 2D mammograms and, therefore, extremely hard to find
These factors have made breast density a core area of focus for radiology, particularly with regard to introducing tailored screening protocol, which can have an impact on both clinicians and patients in terms of the sensitivity of mammography in dense breasts and fatty breasts.
 Dr. Francesca Caumo.
Dr. Francesca Caumo.I have been working on introducing the American College of Radiology (ACR) Breast Imaging and Reporting and Data System (BI-RADS) categories for breast density, so have seen the evolution of, and challenges associated with, establishing breast density protocols.
Currently, our team is assessing breast density, looking at the digital images and assigning density based on the ACR's BI-RADS categories. Although this technique has demonstrated good results for many patients over the years, visual assessment is not always reproducible with different intra- and interreader agreement, which means there is room for argument in how to classify a given patient. Standardizing these assessments with quantitative methods is fundamental to introduce breast density as a risk assessment method.
As a result, a lot of research has been conducted in the radiology industry to develop software for a quantitative assessment that is more reliable and reproducible than the visual qualitative assessment.
New study of 10,000 women
Our department has recently received approval to start a risk-based breast screening study that will follow up to 10,000 45-year-old women over five years. These patients' mammographic densities will be interpreted by two radiologists using the ACR's BI-RADS visual method and also software that will calculate the breast density based on quantitative density measurements. Evaluation of patients' breast density may provide information on their potential breast cancer risk, and it also could lead to establishing the best personalized screening for them.
The current European guidelines for screening mammograms indicate that women should start getting screened for breast cancer at age 50 and continue biennially until age 74, regardless of their breast parenchyma density.3 Right now, even if patients with dense breasts have an increased risk of developing breast cancer and sensitivity of mammogram is lower in their type of breast tissue, specific guidelines are not available to offer further assessment of these individual patients.
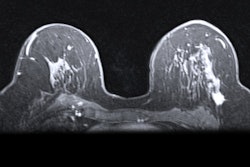
Previous studies have shown that patients with dense breasts have optional screening choices to increase their cancer detection rate. In 2017, the results of the Verona pilot study showed that digital breast tomosynthesis (DBT) identified more cancers in dense breasts compared with full-field digital mammography (FFDM) (12.9 x 1,000 versus 4.5 x 1,000 in BI-RADS C-D).4
At the moment, not all facilities in Italy and other parts of Europe have DBT technology, and it can certainly be costly to introduce it, but it has demonstrated its effectiveness for finding more cancers in dense breasts, making it an investment worth pursuing for facilities in Italy -- and Europe as a whole.
Although ultrasound and MRI options also are beneficial for cancer detection in dense breasts, when patients are screened with DBT and their mammograms come back normal, they can rest assured that they do not need further follow-up. With a uniform approach to prioritize DBT screening for women with dense breasts, clinicians can help increase the chances of early detection for their patients who have breast cancer while also avoiding follow-up for patients who don't.
There is still more to learn about breast density, and there is a clear need for clinicians to have a standardized approach to breast density assessment and tailored screening. Introducing personalized screening will require much effort and investment of resources, yet this will improve patient outcomes and also patient awareness.
Patients' awareness of their personal breast cancer risk may potentially improve compliance toward breast screening, which will benefit not only patients but also clinicians. As technology continues to advance, it should be a key priority for all radiologists and facilities to make an effort to develop and introduce guidelines that can give women with dense breasts the best clinical outcome available.
Dr. Francesca Caumo is a radiologist and the head of the department of breast radiology at Veneto Institute of Oncology (IOV) - Scientific Hospitalization and Treatment Institute (IRCCS) in Padua, Italy.
References
- Dense Breast-info website. http://densebreast-info.org. Accessed 21 February 2019.
- Boyd NF, Guo H, Martin LJ, et al. Mammographic density and the risk and detection of breast cancer. N Engl J Med. 2007;356(3):227-236.
- Recommendations from European Breast Guidelines. European Commission Initiative on Breast Cancer website. https://ecibc.jrc.ec.europa.eu/recommendations. Updated February 4 2019. Accessed 21 February 2019.
- Caumo F, Zorzi M, Brunelli S, et al. Digital breast tomosynthesis with synthesized two-dimensional images versus full-field digital mammography for population screening: Outcomes from the Verona Screening Program. Radiology. 2018; 287(1):37-46.